Updated on 25. April 2022 from Marc Hedemann
Reading time: approx. 15 minutes
Pain in the back – What helps with spinal stenosis
Unfortunately, the ageing process does not stop at the spine, the central axis of the body. It leads to signs of damage that are most pronounced in the mobile sections, i.e. the lumbar and cervical spine. The result is arthrosis, bony growth of the intervertebral joints and also an enlargement of the surrounding ligaments. This narrows the spinal canal, pinching the spinal nerves and possibly the spinal column.
Are you affected and do you have many questions after the diagnosis of spinal stenosis? If you are affected by spinal stenosis, you can read important information below about the causes, signs and, above all, the treatment options.
- Description
- Symptoms
- Shapes
- Causes
- Diagnosis
- Progress & Forecast
- Conventional Medicine Treatment
- Natural & Alternative Therapies
What is spinal stenosis ?
Inside the spine lies the spinal canal (in technical jargon: spinal canal). This structure of bones and ligaments surrounds the soft spinal column and also the nerves that make a journey to the legs. The spinal canal thus forms a bony shell. If the spinal canal is narrowed (stenosis), it is called spinal stenosis. Most often, the spinal canal is narrowed in the area of the lumbar spine (posterior spinal stenosis).
Posterior spinal stenosis is a very common condition in older people. One in five people over the age of 60 has a narrowing of the spinal canal.
Who has spinal stenosis?
- Common disease – approx. 5% of all people, of which (only) 14% are symptom-free
- 80% In The Lumbar Spine = Restricted Back. Spinal Stenosis (80%), Cervical Spinal Stenosis (15%) And Also Thoracic Spinal Stenosis (4%).
- 65% Of Those Affected Have What Is Known As Intermittent Spinal Claudication.
- Gender: ♀= ♂
- Age: Frequency in the 60th to 70th year of life
The spinal canal

The spinal canal runs inside the spinal column. The illustration shows a lumbar vertebra – viewed from the side – with spinal cord (1), spinous process (2), nerve root (3), pedicle (4), intervertebral disc (5) and vertebral body (6). The spinous process points backwards and can be felt and palpated externally. The vertebral body points towards the abdomen.
The spine
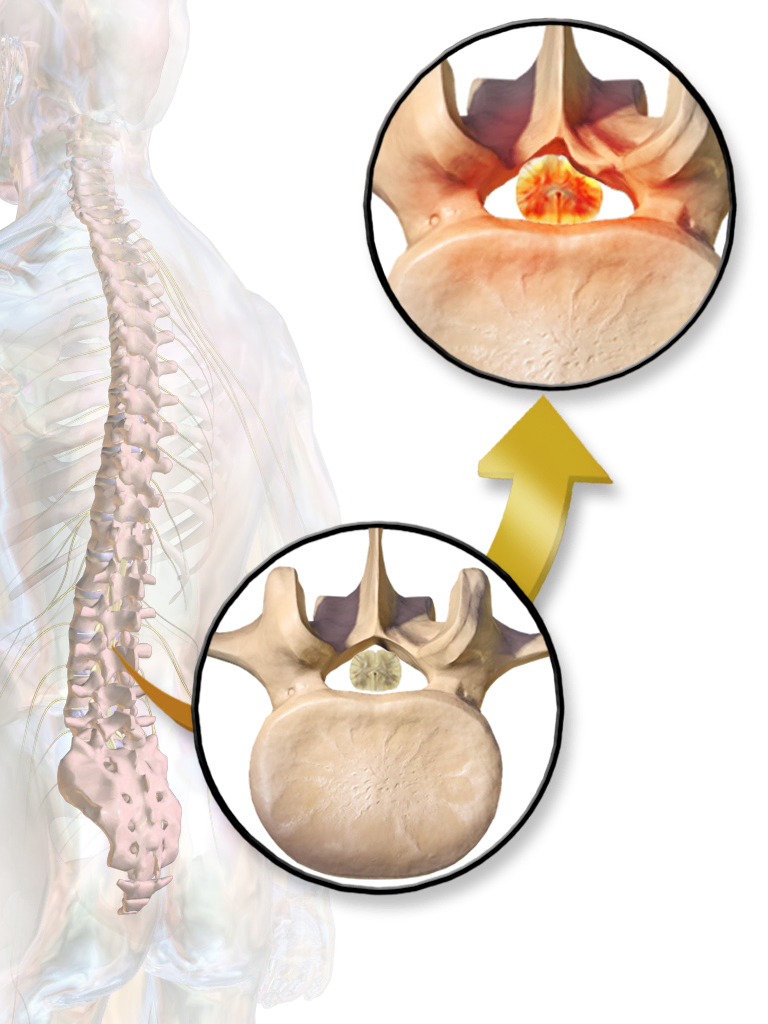
The individual vertebral bodies “stacked on top of each other” form the spinal column and are connected by tiny joints. In the centre of each vertebral body is an opening. The individual openings stacked on top of each other form the vertebral canal (spinal canal). It forms the protective passage for the soft, sensitive spinal column. The spinal cord contains nerve material that transmits stimuli from the brain to the body. Nerves arise at certain points in the spinal column, which then branch out further and, for example, also control the activities of the arms and legs. The cartilaginous intervertebral discs lie between the bony vertebral bodies.
The intervertebral discs cushion certain movements (for example when jumping) like shock absorbers and allow the spine to bend to different sides. The back consists of individual sections: Cervical spine, thoracic spine, lumbar spine, and sacrum and coccyx.
What are the symptoms of spinal stenosis?
Similar to a constricted tube, the flow of nerve impulses is disturbed. For the individual, this means not only neck and back pain as well as leg complaints, but also that longer efforts can no longer be managed or, conversely, that physical performance decreases. This manifests itself in particular in a reduction of the possible walking distance. The person affected has to take frequent breaks from standing or sitting. For this reason, spinal stenosis is also called claudication. In addition, sensory disturbances and even paralysis of the legs can occur.
At the beginning of the disease, the signs and symptoms are non-specific and vary in severity. These non-specific complaints include:
- Back pain in the lumbar region (Lumbago), usually radiating to one side of the legs (lumboischialgia)
- minimised range of motion in the lumbar spine region
- Muscular tension of the tissue in the area of the lumbar spine
If the stenosis progresses further, the following problems are conceivable:
- Sensory disturbances in the legs
- Abnormal sensations in the legs, e.g. shivering, running ants, feeling cold, sucking cotton wool under the feet
- Feeling of weakness in the leg muscles
- Limping caused by pain (claudication spinalis)
- Bladder and/or rectal problems (problems with defecation and peeing or * urinary incontinence).
- impaired sexual function
Different types of spinal stenosis
Claudication spinalis: rapid increase of discomfort in the legs;
The main sign and symptom of this spinal stenosis is a rapid increase in pain in the legs when standing or walking. If one sits down or remains with the upper body bent forward, these regular nerve complaints often subside quickly.
The consequences of these spinal stenoses can vary greatly from person to person.
- Pain in the back (lumbago)
- Complaints that radiate into the legs
- Increased discomfort when walking
- Muscle cramps in the legs
- Immediate relief of discomfort by sitting down or leaning forward for support
- Numbness and coordination problems in the legs
- unsteady gait
- Drawing pain in the front and back of the legs
Signs and symptoms of lumbar spinal stenosis
The most important sign of spinal stenosis is a rapid increase in pain in the legs when standing or walking. If one sits down or supports oneself with the upper body bent forward, these typical nerve complaints usually disappear quickly.
The consequences of lumbar spinal stenosis can vary greatly from person to person:
- Back pain radiating into the legs
- Stiffening of the spine
- Tension of the muscle tissue in the back
- Sensory disturbances in the legs
- Leg muscle weakness, restriction of maximum walking distance due to insensitivity
- Paraesthesia such as formication, shivering, numbness and sensory disturbances in the soles of the feet.
- Loss of control over bowel movements and peeing
- Sexual dysfunction
Signs of spinal stenosis of the cervical spine (C-spine)
Narrowing of the spinal cord of the cervical spine (C-spine) causes signs in the face, shoulder, arms and hands: Patients report severe neck or shoulder pain. Sensitivity as well as control of the hands can greatly decrease. Grasping small objects such as needles is difficult. The disturbance of gross motor skills and endurance in the hands is particularly noticeable in many everyday tasks such as buttoning T-shirts or undoing twist ties.
- Neck pain and muscle tension in the neck
- Radiating as well as partly burning discomfort in shoulders and arms
- Tingling sensations and “formication” in the arms and hands
- Gross motor restrictions
- Weakness of the arm muscle mass
Risk of confusion with external circulatory disorders (pAVK)
Both the type and location of spinal compression can often vary. Accordingly, the signs of the disease, the pain or the activity conditions also vary.
This stenosis pain reduces the maximum possible walking distance: the affected person gets relief by sitting down and resting. Afterwards, the pain subsides again. These signs and symptoms are extremely comparable to external circulatory disorders (pAVK). Complications with various other medical conditions are also quite common, so people with spinal stenosis usually do not get the right treatment. For this reason, spinal stenosis is often confused with shop window disease, pAVD or external arterial occlusive disease.
What causes spinal stenosis?
Spinal stenosis is a physiological narrowing of the spinal canal that results in less space for the nerves and vessels running through it. The causes of this narrowing (stenosis) can be both genetic and acquired over time. Often a mix of different aspects leads to spinal stenosis.
Wear-related changes lead to an enlargement of the vertebral joints (arthrosis) with thickening of the joint capsule and also the surrounding ligaments, which reduces the diameter of the spinal canal. Bulging discs can contribute to further narrowing. The nerves that run in the spinal canal are squeezed and cause the usual discomfort.
In older patients over 50-60 years of age, degenerated intervertebral discs usually cause spinal stenosis. As a result of wear and tear and dehydration (loss of the form-giving internal water pressure), the intervertebral discs lose considerable height. The mantle of the intervertebral discs (annulus fibrosus) bulges forward and can also painfully compress the spinal cord in the spinal canal. The disc space loses height and the vertebral bodies also become hypermobile.
The most common causes:
- Signs of damage: Ossification of the vertebral bodies and the joints between the vertebrae, thickening of the ligaments and joint capsules, bulging of the intervertebral discs, spondylolisthesis.
- Idiopathic spinal stenosis: the spinal canal is narrowed from birth for no known reason
Rarer causes:
- Certain acquired bone diseases (e.g. Paget’s disease).
- Strongly developed hollow back (hyperlordosis)
Genetic spinal stenosis:
In the rarest cases, spinal stenosis is hereditary. In these cases, the bones between the vertebral body and the lateral joint (vertebral joint) are too short. This leads to a narrowing of the spinal canal. The rare hereditary form of spinal stenosis can lead to complaints even in very young patients.
Medical diagnosis of spinal stenosis
In case of persistent pain in the back, heaviness depending on the load or pain in the legs, you must consult your doctor if there is no improvement within 1 – 2 weeks. If tingling in the buttocks or leg persists within a few days.

First, a thorough medical history and a thorough examination of the person are required. Pre-existing problems are also checked. How long have the complaints existed? Where does it hurt? What is the quality of the pain? Is there any paralysis or restriction of movement? Is bladder control or defecation impaired?
A neurological examination is also part of the analysis process and provides information about the extent and location of the spinal stenosis.
The medical diagnosis of spinal stenosis is a difficult area. Important – besides the necessary X-ray examination – is a magnetic resonance imaging (MRI).
The MRI shows the usually regular protrusion of the height-reduced, desiccated intervertebral disc into the spinal canal. Typically, the examining spine specialist discovers the matching stenoses in the vertebral segments L3/L4 or L4/L5. Sometimes several stenoses can be seen. The professional significance of the visible stenoses can only be determined by precisely matching the radiological findings with the results of the neurosurgical assessment. Often conspicuous stenoses are visible in the image even without technical findings or signs.
What radiological indications does the examining doctor pay particular attention to?
- Narrowing of the spinal canal
- Thickening (hypertrophy) of the arthritic facet joints, which are clearly overloaded due to disc shrinkage
- Occurrence of spondylophytes as an indication of segmental instability
- Disc protrusions into the spinal canal as a result of increasing disc desiccation
- Hypermobility (Spondylolisthesis) of the vertebral bodies (captured in images the flexed and extended position of the back)
- Thickening of the longitudinal ligament of the spine (Ligamentum flavum)
After a precise neurological and neurosurgical diagnosis, a possible involvement of the vascular system due to peripheral arterial occlusive disease (PAVD) must also be excluded.
Course & Prognosis of spinal stenosis
Spinal stenosis usually progresses very slowly, even if it is not treated. Depending on the cause, the disease can also progress in extremely different ways. The discomfort caused by the strain on the nerves may persist, diminish with certain movements or over time, or recur frequently. Occasionally, the signs and symptoms even decrease with age, when the spine becomes less mobile. This is because the nerves are then irritated much less often, so movement-related pain is less frequent.
Sometimes, however, spinal stenosis progresses acutely: for example, if disc cells shift (prolapse, prolapse), if joint inflammation leads to capsule swelling or if fluid accumulates near the nerve pathways, the signs and symptoms of spinal stenosis can suddenly worsen. Often one side of the body is particularly affected.
In general, spinal stenosis can be treated well with conservative treatment methods in most cases, so that those affected can lead a relatively symptom-free life.
Traditional therapy: physiotherapy and medication
As a rule, conservative therapies are used first, especially physical treatment (physical rehabilitation) and medication for the symptoms.
Physical rehabilitation
The aim of physical rehabilitation is to train the back and abdominal muscles, as a solid muscle mass supports the back and can reduce the pressure on the back. This is to reduce the hollow cross position of the lumbar spine so that the spinal canal expands. Especially the deep muscle mass has to be taken care of during the therapy: The so-called musculi multifidii are small muscle masses that provide security to the spine. They can best be released through unique balance as well as resonance training.
Medication
Medication supports physical therapy by relieving pain and protecting the muscles from cramping. If the pain is very severe, an injection of an anaesthetic as well as an anti-inflammatory cortisone directly into the affected nerve origin can provide relief.
Relaxation techniques
Additional relief can be achieved through relaxation techniques.
The cause of the complaints, especially the current bony narrowing of the spinal canal, cannot be reversed by physical rehabilitation. However, regular training can bring about lasting relief of the symptoms.
If surgery is required
Surgical therapy involves widening (decompression) of the spinal canal. Surgical intervention is only suggested if the pain can no longer be relieved with conservative measures.
In this case, the doctor must not make his decision based on X-rays alone, but must be guided by the actual signs and symptoms. It is not uncommon for the X-rays to look negative but for the affected person to have minimal problems. Whether an operation makes sense depends above all on how great the suffering of the affected person is and whether he or she is also putting nerves at risk.
19 Everyday Tips And Natural Therapies For Sufferers
Food against back pain
Eating against back pain – Is this possible? Pain in the musculoskeletal system is associated with inflammatory processes in the body in numerous situations. However, we cannot eat ourselves pain-free. But there are foods that have an anti-inflammatory effect, strengthen connective tissue and support bone and muscle function. In this way, you reduce your risk of spinal stenosis and subsequently persistent neck and back pain.
1. Probiotics
A sufficiently high diversity of microorganisms in the digestive tract is essential for the health of our intestines and the absorption of nutrients. Probiotic foods are mainly found in sour milk products, natural yoghurt and also sauerkraut. Bacterial cultures can additionally be supplied to the body via food supplements.
EXCEPT: Bacterial stresses are linked to serotonin metabolism and thus also influence the production of happiness hormones! So you eat twice against neck and back pain.
2. Acid-base Balance
A balanced acid-base balance not only keeps the gut healthy, but also reduces the risk of inflammation. For this reason, you should include alkaline foods such as vegetables, potatoes, fruit and also herbs in your diet. On the other hand, avoid grains, meat and fish (except omega-3 acids). Avoid alcohol, sugar and coffee as much as possible in your diet for neck and back pain.
3. Omega-3 Fats
Foods that contain omega-3 fats relieve back pain caused by inflammation. These are fatty fish such as salmon, herring or even mackerel. High-quality oils with anti-inflammatory fats consist of linseed oil, walnut oil, rapeseed oil as well as fish oil. One of the most important pieces of advice for the diet for neck and back pain!
4. Vitamin C
Perhaps the best known vitamin (vitamin C) is essential for back wellbeing because it develops collagen, which nourishes helpful connective tissue. It is found in fruits, vegetables, especially collard greens and green vegetables, and herbs.
5. vitamin D
Vitamin D promotes the absorption of calcium from food in the intestine. It is found in fatty fish, dairy products, eggs and also certain mushrooms such as porcini, morels and also mushrooms. However, vitamin D is converted in the body with the help of the sun. Simply put, if the skin does not get sunlight, vitamin D deficiency is inevitable and calcium absorption in the intestine is also stopped.
6. vitamin K
Vitamin K forms healthy proteins that we need to build and strengthen our bones. Green vegetables as well as salads contain the largest amount of this light-sensitive vitamin and should therefore not be missing from the diet for back pain. Please note: Store vitamin K-rich foods in the dark!
7. Calcium
Osteoporosis, bone loss, increases the risk of vertebral fractures and thus also of persistent back pain. Calcium-rich foods such as dairy products, especially hard cheese, green vegetables such as kale, fennel, leeks, spinach and broccoli, as well as mineral water enriched with calcium, ensure the strength and stability of the bones.
8. Magnesium
Das Mineral ist entscheidend für die Funktion der Muskelmasse. Die Spitzenreiter unter den magnesiumreichen Lebensmitteln sind Weizenkleie, Kürbis- und Sonnenblumenkerne. Aber auch Zartbitterschokolade, Cashew- und Erdnüsse sowie Vollkornmehl, Haferflocken und auch Bananen liefern viel Magnesium und sind ein fester Bestandteil in der Ernährung gegen Schmerzen im Rücken.
The mineral is crucial for the function of muscle mass.
Sie greifen Schadstoffe im Körper an und schirmen die Zellen vor den freien Radikalen ab – Antioxidantien dienen als eine Art “Reiniger” im Mikroorganismus. Beliebte Vertreter sind Gemüse, Früchte, vor allem aus natürlichem Anbau, Kräuter, Nüsse sowie Samen.
10. Mood Enhancer
Foods rich in tryptophan, a precursor of the happiness hormone serotonin, lift mood and reduce pain perception. Nuts, especially cashews, seeds, bananas and dark chocolate have the highest amount of it.
Eating against back pain does not only mean to eat healthy, but also to eat pleasurably, varied and fresh!
11. Water And Natural Teas
The human organism has a water content of 75 percent. If we do not supply it with sufficient fluid – 2 to 2.5 litres per day – the intervertebral discs remain undersupplied and do not give the spine the necessary flexibility.
12. Plant Power Against Back Pain
A 2014 published Cochrane study investigated phytotherapeutics for the relief of back pain. According to this study, extracts of willow bark (salicis cortex, from Salix alba) standardised to 240 mg salicin were effective in the short term without significantly inhibiting platelet aggregation. The root of devil’s claw (from Harpagophytum procumbens), standardised to 50 mg or 100 mg harpagosides, also performed significantly better than placebo. Taking both plants produced results comparable to 12.5 mg of rofecoxib. Willow bark is approved by the European Medicines Agency (EMA) for ” recognised use based on available efficacy and safety and security studies ” for the temporary relief of low back pain. The EMA lists devil’s claw only as a traditional medicine for minor joint pain. Also because of the lower quality of research, the NVL refrains from recommending devil’s claw, but allows willow bark for the treatment of persistent neck and back pain. There is no pharmacy-only preparation made from willow bark on the market.
Capsaicin, the pungent substance from chilli (Capsicum annuum), desensitises the pain-conducting fibres after an initial burning sensation. Externals containing capsaicin can be used in self-medication in combination with physical activation for low neck and back pain; 2 studies in patients with persistent symptoms and one in people with acute pain support this, according to the Cochrane review. An EMA monograph confirms the ” recognised use ” of capsaicin for temporary relief of muscle pain. Comfrey (Symphytum officinale) comes in ointment form and was also more effective than placebo as a baseline in a study of 120 patients with reduced neck and back pain. However, due to the paucity of evidence, the authors of the NVL tend to advise against using a cream containing comfrey for non-specific reduced back pain.
13. Heat/cold Therapy
- Heat therapy, where you use a hot pillow, warm towel, warm bath or other heat source to relax rigid muscles.
- Cold treatment, where you place an ice pack or ice wrapped in a towel on swollen areas to relieve swelling and pain.
14. Yoga Exercises / Tai-chi / Qigong
Light movement treatments. Yoga exercises, Tai-Chi and also Qigong train body awareness, the adaptation of movement patterns as well as the improvement of movement psychronisation with different focuses. Although not originally established as a back therapy, these exercise-based mind-body approaches have proven themselves in practice for the treatment of persistent, sometimes acute neck and back pain. For yoga in particular, there are now numerous scientific studies available.
15. Acupuncture
Permanent or regularly recurring neck and back pain can have a number of causes. Usually, degenerative changes in the spine are the cause, such as herniated discs, problems in the lumbar spine (LS) or spinal stenosis. In the following, acupuncture can be used to alleviate the complaints.
First, a timeless anamnesis is taken, i.e. the individual signs are carefully checked. Before an acupuncture treatment, an anamnesis according to the concepts of Traditional Chinese Medicine is taken in addition to the conventional medical examination. This includes the tongue diagnosis and also the pulse diagnosis; they provide information about essential details for the acupuncture treatment. As a rule, ten acupuncture sessions are spread over a period of six weeks.
Since the effectiveness of acupuncture in the treatment of knee and neck and back pain has been proven by numerous studies, the therapy is covered by statutory health insurance in Germany.
16. Massage Therapy
Gently massaging a sore or tight muscle is one of the most reliable ways to loosen it up and also eliminate pain. In a research study it was found that massage therapy along with usual treatment:
- reduces the pain in the back
- Improves the function of the back
- Minimised the use of anti-inflammatory drugs
- Requires fewer days of absence from the workplace

Fascia rolling massage: When rolling, the fascia tissue is pressed, so to speak, so that it can subsequently absorb fresh, nutrient-rich water. This loosens adhesions and the fascia layers can move much better in the tissue. To achieve this result, you should very gradually roll in one direction (towards the heart) with constant strong pressure.
17. Stretching

You proactively stretch into the pain during the workout and hold each position for about two to two and a half minutes. In this way, you offer your muscles and fasciae the necessary adaptive impulses and give them enough time to give in. Make sure that you do not exceed your personal comfort level. Stick to it and train 6 days a week if possible.
18. Take A Relaxing Magnesium Bath
Epsom salt or magnesium sulphate overcomes the skin and penetrates directly into the aching muscle mass. A 20-minute bath can help relieve sore back muscle tissue, especially after exercise.
If you take an Epsom salt bath, make sure the water is warm. Hot water can cause muscle swelling and cold water can cause muscle tissue spasms. The Arthritis Structure recommends a temperature between 92 and 100 ° F (33 and 38 ° C). Temperatures above 40 ° C are discouraged, especially if you suffer from heart problems.
You can also enhance the soothing effect by taking a tennis ball or other rubber ball of similar size into the tub with you. Place it on your lower back or the middle of your back and move it from side to side. The effect is like a back massage and also loosens tense muscle tissue.
Another benefit of Epsom salt is that it is good for your skin. Epsom salt can remove dead skin cells, soften the skin and relieve itchy spots.
19. Spinal Stenosis: 3 Workouts Against The Pain
Exercise 1: Stretch backwards
In this exercise you perform a hyperextension of the spine from bottom to top. Are you unsure because you are standing unstably? No problem: hold on to a stable table or chair for safety.

1. First Place Your Hands At The End Points Of Your Buttocks. Now Press Your Groins Forward Even More And Additionally And Lean Backwards. Keep Your Head Straight For The Time Being.
2. Next You Want To Achieve A Hyperextension Of The Chest. To Do This, Open The Shoulders And Pull The Chin Back.
3. Now Also Stretch Your Head Over And Let It Fall Slowly And Thoroughly Backwards. Your Upper Body Now Forms An Even Arc.
4. Inhale And Exhale Deeply, Strengthening The Stretch With Each Exhale By Pushing Your Groin Even Further Forward.
Very gradually leave the stretching position and straighten up: first the head, then the thoracic spine and finally the lumbar spine.
6. Now Think Of The Counter Posture: Make A Hollow Back And Bend Forward As Well. Support Yourself With Your Hands On Your Thighs And Stay In The Hollow Back As Long As Possible. Then Become Rounder In The Back And Pull The Head Down In Front. To Do This, Place Your Hand On The Back Of Your Head And Press Your Chin Towards Your Breastbone.
This stretches the entire back up to the cervical spine. Now gradually straighten up and release the stretch.
Exercise 2: Lateral stretching exercises to the back

1. First Stretch The Arms Out Flat To The Side. Keep Your Hips Straight And Turn Your Belly Button To The Left. Try To Rotate Only The Lower Part Of Your Spine And Also Keep The Rest Of Your Body Straight.
Do the same with your sternum. Keep your pelvis straight as you push it to the left.

2. Now Move Both Arms To The Left As Far As Possible. Bend The Right Arm To Make Sure You Keep Them Parallel.
3. Finally, Also Turn Your Head Increasingly More To The Left And Look With Your Eyes Parallel. Strengthen The Stretch With Each Exhalation By Breathing Deeply In And Out.
4. Then Slowly Come Forward Again And Do Exactly The Same On The Right Side.
5. When You Reach The End, Align Your Upper Body Forward Again And Let Your Arms Hang Freely.
Exercise 3: Lateral stretching exercises
In this exercise you stretch your hips and also your flanks. Make sure that your upper body does not fall forward or backward, but maintains this axis.

1. Stretch Your Right Arm Upwards And Bend It To The Left Over Your Head. At The Same Time Push Your Right Hip As Far As Possible To The Right. At The Same Time Bend Your Upper Body To The Left And Push Your Left Leg Down With Your Left Hand.
Next, turn your head to the side. It is very important that you keep it straight and look forward, otherwise you will twist your cervical spine. Both your head and your arm are now pulled to the left.
3. After Reaching The Final Position, Inhale Deeply And Exhale Again, Increasing The Stretch With Each Exhalation. Then Gradually Correct Your Upper Body.
4. Then Stretch The Other Side, Starting With The Left Arm Stretched Over The Head To The Right. Keep To The Sequence Described Above.
Repeat the exercises 3 times if necessary.
FAQ
Is spinal stenosis dangerous?
Spinal stenosis usually means a considerable restriction of the quality of life. The complaints have usually existed for a long time, and those affected have also often been struggling with neck and back pain for several years, which gradually intensifies and radiates into the legs.
What are the signs and symptoms of spinal stenosis?
In addition to the typical pain when walking and standing, spinal stenosis often triggers other symptoms: at the beginning of the disease, mainly tingling, weakness and also numbness in the legs. In later phases, also urinary and faecal incontinence as well as erectile dysfunction.
What is high grade spinal stenosis?
Normally, spinal stenosis in the cervical spine is associated with an altered movement pattern. You also find it difficult to button T-shirts or grasp small objects. Paralysis symptoms and also sensory disturbances are generally unusual and are signs of extreme narrowing.
Can spinal stenosis regress?
Even without treatment, spinal stenosis does not necessarily progress: the signs can remain the same or regress for a very long time. To alleviate the symptoms, spinal stenosis is usually first treated conservatively with physiotherapy and painkillers.
What should be avoided in spinal stenosis?
The hollow back narrows the spinal canal. Slight bending of the legs as well as supporting the upper body when standing flattens the hollow back, the spinal canal widens. The hollow back is reinforced by high heels and overhead work.
How to sleep with spinal stenosis?
The most suitable resting position is on the side with the knees slightly bent, as the spine then takes up its natural curvature. The prerequisite is a pillow that is as point-elastic as possible and supports the body effectively, especially in the shoulder and hip area.
Is walking good for spinal stenosis?
As a rule, the patient is relieved of the pain of the spinal stenosis immediately after the operation and the walking distance increases after a short time, so that the affected person can quickly walk again without major restrictions.
What diet for spinal stenosis?
Front-runners among the foods containing magnesium are wheat bran, pumpkin and sunflower seeds. But dark chocolate, cashews and peanuts, together with wholemeal flour, oatmeal and bananas, also contain plenty of magnesium and are a traded component in the diet against neck and back pain.
What sporting activity for spinal stenosis?
Especially sports that are performed with a slight upper body inclination, such as cycling, backstroke or Nordic walking, benefit the back channel.
What vitamins for spinal stenosis?
Vitamin D
It has even been medically proven that many spinal stenosis patients have a vitamin D deficiency. Symptoms of vitamin D deficiency include stunted growth, fatigue, headaches and also reduced muscle tone and stamina. This manifests itself in an awkward posture.
The B-Vitamine
Effective especially for nerve complaints. Typically triggered by diabetes, but then also “sciatica”, neck complaints (because the nerve root at the spine is compressed or inflamed), or triggered by arthrosis, i.e. knee as well as hip complaints.
ICD codes for this disorder: F20 | F20.1 | F20.2 | F20.3 | F20.4| F20.5 | F20.6 | F21
ICD codes are internationally valid codes for medical diagnoses. They can be found, for example, in doctors’ letters or on certificates of incapacity for work.
The web content of ÁYIO-Q.com is for your information and in no case replaces a personal consultation or treatment by a qualified physician. The contents of ÁYIO-Q.com cannot and must not be used to make independent diagnoses or for self-medication.
Sources:
- Daniel C. Cherkin, PhD, Karen J. Sherman, PhD, MPH, Janet Kahn, PhD, Robert Wellman, MS, Andrea J. Cook, PhD, Eric Johnson, MS, Janet Erro, RN, MN, Kristin Delaney, MPH, Richard A. Deyo, MD, MPH, A Comparison of the Effects of 2 Types of Massage and Usual Care on Chronic Low Back Pain, A Randomized, Controlled Trial, https://doi.org/10.7326/0003-4819-155-1-201107050-00002
- Oltean H et al. Herbal medicine for low-back pain. Cochrane Database Syst Rev 2014;12:CD004504. DOI: 10.1002/14651858.CD004504.pub4,
- Saper RB, Lemaster C, Delitto A, et al. Yoga, Physical Therapy, or Education for Chronic Low Back Pain: A Randomized Noninferiority Trial. Ann Intern Med. 2017;167(2):85-94. doi:10.7326/M16-2579