Updated on 17. February 2022 from ÁYIO-Q Redaktion
Reading time: approx. 15 minutes
The bottom line: The right treatment at the right time
Sudden – Severe and stabbing pain in the back radiating to the legs or arms. A tingling sensation in the toes or fingers. Paralysis or loss of sensation in the arm or leg. The diagnosis? A so-called herniated disc.
A disc prolapse (herniated disc) occurs most often in people between 30 and 50 years of age. It often causes no discomfort. But it can also cause severe back pain, numbness and even paralysis – in which case it is important to act quickly. Read all about the symptoms, examination and treatment of herniated discs here!
- Description
- Symptoms
- Causes
- Frequency
- History
- Diagnosis
- Treatment with orthodox medicine.
- Rehabilitation
- 12 Natural Therapies
What is a herniated disc?

Many people suffer from back pain from time to time. In most cases, the cause cannot be determined exactly. However, if the pain radiates down the leg to the foot, this may indicate a herniated disc.
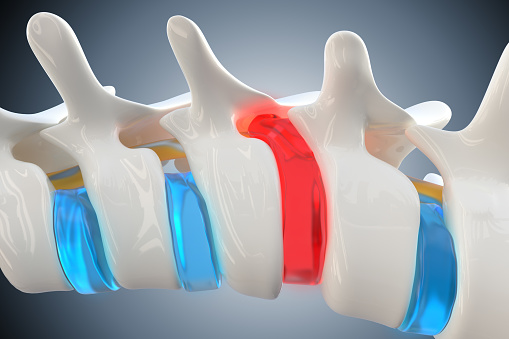
The intervertebral discs lie between the vertebral bodies of the spinal column. They consist of an elastic mantle of cartilage fibres and a gel-like core (gelatinous core). In the case of a herniated disc, disc tissue protrudes between the individual vertebral bodies. This “prolapsed” tissue can press on and irritate nerves in the area of the spine.
A slipped disc can be very unpleasant. However, for most people, the discomfort subsides on its own within six weeks. In addition, not every herniated disc causes discomfort.
What are the symptoms of a herniated disc?
A herniated disc can suddenly cause a sharp, “shooting” pain. In the case of a herniation in the cervical spine, the pain can radiate into the arms. Herniated discs in the lumbar spine are the main cause of sciatica (colloquially “sciatica”). Pain that radiates into a leg and foot is called sciatica. A herniated disc can also manifest itself as pain in the lower back in addition to the typical radiating pain.
Rarely, in addition to pain, sensory disturbances in the buttock area or paralysis symptoms occur. These symptoms indicate a serious problem such as nerve damage. If bladder or bowel function is also disturbed, immediate treatment is needed. This so-called cauda syndrome is a medical emergency.
Not every herniated disc is associated with symptoms. This is shown by studies in which adults without back pain were examined using magnetic resonance imaging: In more than 50 out of 100 people examined, there was a herniated disc. In about 20 out of 100 examined, the intervertebral disc was already more severely damaged or tissue had even leaked out without causing any symptoms.
What are the causes of a slipped disc?
In most people, slipped discs are the result of wear and tear. Over the years, the resilience of the intervertebral discs decreases: They lose fluid and become brittle and fragile. Such changes are part of the normal ageing process – which, however, varies from person to person. In very rare cases, an accident or serious injury can also lead to a slipped disc.

Cross-section
the
spine
If the spinal column is no longer able to cushion stresses so well, a herniated disc can occur. The pain probably occurs because the disc tissue presses on a nerve in the area of the spinal cord.
When bulging or leaking tissue irritates a nerve root in the lumbar spine, it often leads to the typical sciatic pain. The nerves that run in the spinal canal (spinal nerves) connect in the pelvis to form the sciatic nerve, which supplies the legs. An irritated sciatic nerve can cause tingling and numbness in addition to pain.
Experts distinguish between the following degrees of severity:
- The intervertebral disc bulge (protrusion): Here, the intervertebral disc is bulging out between the vertebral bodies. However, its outer shell is still undamaged.
- Extrusion (protrusion): In extrusion, the outermost shell of the intervertebral disc is torn, allowing disc tissue to escape. However, the escaping tissue is still connected to the disc.
- The sequestering disc herniation (sequester): The disc tissue that has leaked into the spinal canal and is no longer in direct contact with the disc is called a sequester.
This classification says little about which symptoms occur and how severe they are. However, the type of herniated disc can be important for the choice of treatment and the course of the disease.
Frequency of disc herniation.
It is estimated that between 1 and 5% of all people experience lower back pain at some point in their lives due to a herniated disc. Disc problems are more common in the over-30 age group and are about twice as common in men as in women.
Progression of the herniated disc
Pain and movement restrictions as a result of a herniated disc subside on their own in about 90 out of 100 people within six weeks. It is thought that over time the human body breaks down a certain amount of the leaked tissue or that it shifts so that it no longer irritates the nerves.

A painful herniated disc can be very different: The pain can occur suddenly and quickly disappear on its own. Some people have permanent pain over a longer period of time, others have pain in episodes.
If the symptoms last longer than six weeks, it is unlikely that they will go away on their own.
How does the doctor diagnose a herniated disc?
The general practitioner’s office is usually the first place you go when you are ill or need medical advice for a health problem.
In order to clarify acute back pain, a conversation and a physical examination are usually sufficient. X-ray images are not very informative for the diagnosis of a herniated disc, as they are not very meaningful: Even in many people without symptoms, disc damage can be seen on the X-ray image. Further examinations with other imaging methods such as magnetic resonance imaging is rarely necessary, namely when:
- Paralysis symptoms occur in one or both legs,
- the bladder or bowel function is disturbed,
- the pain is hardly bearable despite treatment,
- severe symptoms persist for weeks despite treatment, or
- there is a suspicion that another disease is causing the pain, e.g. a tumour.
In the case of back pain, the doctor often has good reasons not to order extensive examinations: Imaging examinations can reveal a supposed cause for low back pain that actually has nothing to do with the symptoms. Such a misdiagnosis can in turn lead to unnecessary treatment that can even cause harm.
Treatment of a herniated disc with conventional medicine
Even severe sciatica pain can subside on its own over time. Until then, various pain-relieving treatments can help to ease the discomfort. The goal is to stay as active as possible. However, treating the pain does not lead to a faster recovery. The body usually does most of the work on its own.
If severe sciatic pain due to a herniated disc lasts longer than six weeks, surgery may be an option to relieve the affected nerve. Surgery is also always necessary if the nerves are so badly affected that the bladder or bowels no longer function properly, or if certain muscles are very weakened. However, this only happens rarely.
Rehabilitation for a slipped disc
The aim of rehabilitation is to reduce the discomfort and impairment caused by a slipped disc, to strengthen the trunk muscles and thus to improve the stability of the spine.

Rehabilitation can include back school, stretching and relaxation exercises, strength training and other measures. It is suitable for people who are so severely impaired by their back pain that they cannot work or are restricted in their everyday life. Aftercare can also be useful after an operation.
12 Natural Therapies & Remedies for a Herniated Disc.
Since alternative measures were developed more for prevention and permanent improvement or healing, they will naturally not provide the preferred quick relief in the case of a herniated disc.
Nevertheless, they can do a lot to ensure that this one slipped disc is not followed by others.
Sufficient exercise, attention to regular minutes of relaxation and adequate fluid intake are the basic prerequisites for keeping the intervertebral discs healthy and balanced or for restoring them to health.
Ausreichend Bewegung, die Beachtung von regelmäßigen Entspannungsminuten sowie eine ausreichende Flüssigkeitszufuhr sind die Grundvoraussetzung dafür, dass die Bandscheiben gesund und ausgeglichen bleiben oder wieder gesund werden.
Whether you are currently affected by a slipped disc, suffer from persistent back pain or simply want to keep your back healthy and balanced – your spine will benefit from our suggestions in any case.
And since these are alternative procedures, it is of course not only your back that benefits from the positive effects, but your whole body. Here we give you some measures to avoid it:
1. Enough fluid intake.
As is now known, the intervertebral discs release fluid during stress, which they can absorb again during periods of rest. However, the absorption of fluid can only take place if there is no permanent lack of fluid in the organism.
If this is the case, the intervertebral discs “dry out” and the gelatinous core also loses considerable substance, so that the fibrous ring is subject to increasing pressure.
If the fluid deficit persists over a longer period of time, the condition of the intervertebral discs deteriorates. They become inflexible and lose their resilience, so that a herniated disc is inevitable.
You can prevent this development by drinking sufficient amounts of still water every day. Consume smaller amounts throughout the day so that the water can reach the cells of the intervertebral discs and not just flush the kidneys, as is the case with larger amounts at the same time.
2. Good nutrition and exercise
When a slipped disc is the result of nutrient deficiency and lack of exercise
Normally, all body organs are supplied with oxygen as well as nutrients and important ingredients via the blood. However, no blood flows through the intervertebral discs. Therefore, these important substances must be absorbed by the interstitial fluid so that they can reach the cells during the resting phases when the intervertebral discs become saturated with fluid.
This process naturally requires a sufficient supply of nutrients and vital substances through appropriately prepared food.
The use of nutrients and vital substances in the cells always leads to metabolic residues, which are eventually released back into the interstitial fluid in times of stress and restlessness so that they can be delivered to the laxative organs and excreted.
In this way, the interstitial fluid not only covers the intervertebral discs’ need for fluid, but also supplies them with all the nutrients and vital substances and at the same time enables the removal of mobile waste.
However, in order for the intervertebral discs to be optimally supplied and additionally to be able to ensure the disposal of metabolic residues, they depend on a balanced ratio of activity and rest.
If the intervertebral discs lack sufficient rest, nutrients and vital substances cannot be absorbed in sufficient quantities, and if this deficiency persists over a longer period of time, they begin to atrophy.
Incidentally, the very best rest for the intervertebral discs is not resting. Rather, the intervertebral discs like the lying position, in which they can absorb a particularly large amount of fluid.
A constant lack of movement is just as unpleasant for the intervertebral discs as the absence of recovery phases, because the lack of movement means that they can no longer sufficiently break down their metabolic residues. As a result, the cells virtually suffocate in waste. They become inflamed and the absorption of nutrients and vital substances is also no longer possible.
Of course, the intervertebral discs also degenerate and it is again only a matter of time before the herniated disc occurs.
3. Deacidification
In the case of a slipped disc as a result of chronic hyperacidity
A persistent over-acidification of the body can additionally favour a slipped disc. This is caused, among other things, by a harmful, over-acidifying diet (lots of fast food, too much sugar, meat, dairy products and also gluten-containing cereals), an excess of coffee, nicotine and also alcohol, constant stress, lack of exercise or other strongly acid-forming variables.
The neutralisation of all acids formed in excess is crucial for our body. Therefore, in an overacidified state, it needs large amounts of base-forming minerals such as calcium, magnesium, salt, potassium and iron because they can counteract the corrosive acids.
If the required minerals are not supplied in sufficient quantities through the diet, the body has to turn to its mineral stores to restore the acid-base balance, which inevitably leads to a mineral deficiency.
Deacidification avoids slipped discs
The first and most important step to deacidify the body is to change your eating habits. Therefore, from now on, abstain from highly acid-forming foods and drinks and offer your body important substance-rich, alkaline-surplus foods instead.
You can read all the essential details about the alkaline-surplus diet at the following link: Alkaline diet – how it works
As soon as the first positive results of your dietary change become apparent, we advise an additional measure that reinforces the already initiated deacidification process.
This includes drinking a strongly alkaline fluid, which also has the ability to dissolve acids out of the cells so that they can also be excreted in the urine.
In this way, besides the deacidification of the body fluids, a deacidification of the cell interior takes place at the same time.
4. Calcium
The calcium store is used up first
Calcium is a mineral that is present in larger quantities in the body compared to various other minerals. It is found mainly in the bones and teeth, but also in the intervertebral discs. So this is where the body first begins to plunder its stores. If the over-acidification cannot be stopped in time, the intervertebral discs also gradually lose calcium. As a result, they shrink and also lose their elasticity.
Comparable to water deficiency, chronic hyperacidity is also associated with deterioration of the intervertebral discs. A diet rich in bases and an overall healthy and balanced lifestyle reduce the acidity considerably, so that these two elements play a really essential role both in prevention and in existing intervertebral disc problems.
You can find out more about how to support your body in deacidification later in this post.
5. Stress reduction
When a slipped disc is a result of stress
Permanently stressful scenarios contribute significantly to the over-acidification of the body. But this is not the only problem, because in difficult times the entire skeletal and back muscle tissue is also under extreme tension.
This is because in primeval times, challenging scenarios served precisely to prepare oneself optimally for a fight or a journey. Today, however, no one fights under difficult circumstances any more, at least not physically. And no one flees any more either. So the muscle masses wait in vain for the right action and eventually cramp up, especially if the tension is permanent, i.e. chronic. The result is chronic back pain.
It is therefore immensely important to get rid of the constant faulty tensions in the body as quickly as possible. This can be achieved through frequent and sufficient exercise as well as targeted relaxation techniques, as the mixture of both methods immensely reduces the dangerous effects of tension on health.
For the basic protection of the back – including the intervertebral discs – it is advisable to walk as often as possible on the balls of the feet and not on the heels. This supposedly round gait relieves the spine enormously, creates a light body feeling, puts you in a good mood and makes stress disappear in no time. You can read below how the whole thing works exactly.
6 Intestinal cleansing and strengthening with probiotics
In case of a slipped disc due to a disease of the digestive tract.
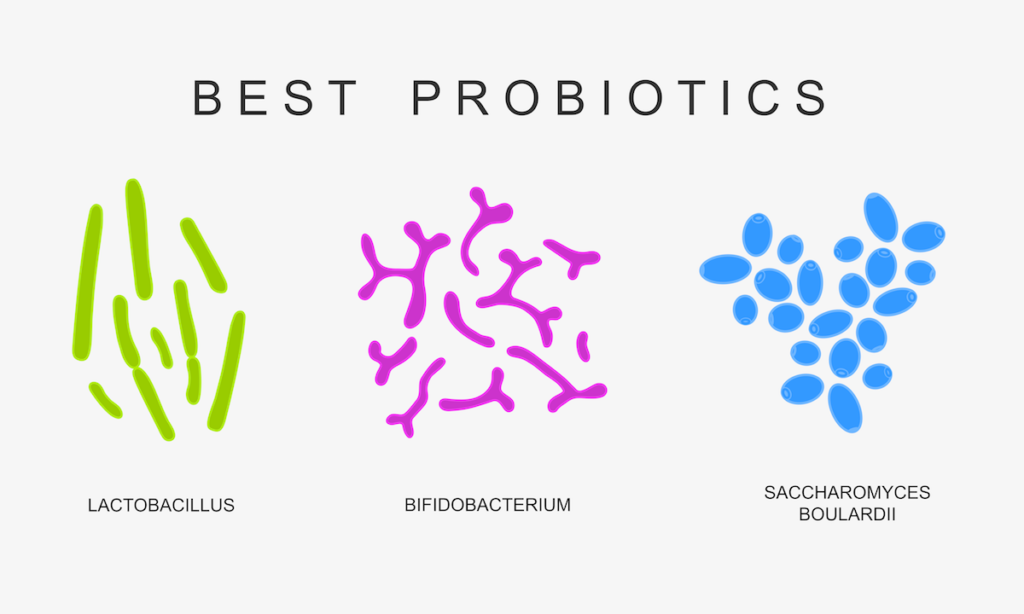
The digestive tract can also be involved in the development of a herniated disc – especially if there is already a persistent intestinal inflammation such as Crohn’s disease or ulcerative colitis.
Anatomically, the digestive tract is in close proximity to the prominent trunk and back muscles as well as the lumbar spine and hip flexor. Therefore, these areas are particularly at risk for persistent inflammation of the digestive tract.
Persistent intestinal swelling leads to constant damage to the sensitive intestinal mucosa. Tiny tears develop in the intestinal wall where the inflammatory processes can eventually spread to the neighbouring muscle groups.
Muscle tension occurs in the affected areas, which is accompanied by a shortening of the supporting longitudinal ligaments and causes the vertebral bodies and also the intervertebral discs to become unbalanced. If the shortening of the tendons finally presses on the spinal nerves running there, agonising movement restrictions can be the result.
If this problem persists over a long period of time, the coarse ring can eventually be broken through by the irreversible pressure of the gelatinous core, leading to a herniated disc.
Even seemingly unspectacular bowel problems, such as a permanently distended abdomen or a permanently overfilled bowel, can be the cause of persistent neck and back pain, because the overstretched bowel can change the natural position of the vertebrae. This can lead to a vertebral displacement, which does not yet trigger a herniated disc, but definitely contributes to severe discomfort in the lumbar region.
Cleanse your intestinal tract for disc problems
A normal cleansing of the digestive tract is important for everyone and for this reason, of course, it is typically recommended for everyone. However, if you already have a chronic bowel disease or incessant digestive problems and your back triggers additional discomfort, then performing a colon cleanse is undoubtedly important.
A colon cleanse is neither an elaborate nor a complex task. Rather the opposite! You can do the colon cleanse yourself in the comfort of your own home. It is really easy to use and does not disturb your usual daily routine in any way.
You will quickly feel the positive results of a cleansed bowel.
7. Back School – Physiotherapy – Chiropractic
In the case of a slipped disc due to malposition
The spine is responsible for our support and thus our posture, while the intervertebral discs take on a buffer function by absorbing loads. It is therefore obvious that permanent bad posture and the resulting one-sided, constant overloading of the spine must in time lead to back problems.
These include irreversible sitting in front of the computer or TV, walking incorrectly, and possibly also lying inaccurately due to a bad bed mattress.
The sufferer is made aware of his “misbehaviour” by agonising body signals in the area of the cervical, thoracic or dorsal vertebrae, which cannot be overlooked.
In order to bear the pain, most of those affected first resort to pain-relieving medication to be able to move at least halfway. But of course this is no solution, because the pain keeps coming back, so that eventually a doctor has to be consulted.
The doctor is of course additionally concerned with restoring his patient’s pain-free ability to move as quickly as possible. He therefore looks at the signs and symptoms and gives the patient useful tips, such as paying attention to posture, not lifting heavy, keeping the affected area snug, attending a back school, etc. Sometimes this can already bring about a significant improvement.
Sometimes a significant reduction of symptoms can already be achieved in this way, but inevitably a purely symptomatic treatment cannot lead to lasting success because possible causes, such as the over-acidification of the body or a persistent intestinal disease, are not taken into account in this treatment technique.
In addition, there is a very important aspect that is completely disregarded: the subconscious.
8 Relaxation Exercises – Meditation – Mental Balance
When a slipped disc is caused by mental overload
Since both the body and the psyche are completely interconnected, the back, like any other part of the body, naturally always reflects a mental style.
The spine is responsible for our outer posture, our physical resilience and our physical versatility. On a psychological level, the current state of the back reflects our inner posture, our psychological resilience and our psychological flexibility.
Therefore, it must be questioned again and again which psychological concern is behind the physical symptomatology.
The concrete question in the case of a herniated disc is: What is this illness, this posture or this discomfort trying to tell me?
To find the best answer as quickly as possible, the following additional considerations can be very helpful:
- Who or what (what scenario) is putting me under so much stress?
- At what point should I rethink my inner attitude?
- What about my sincerity?
- Am I well-founded and can I defend my opinion?
- Where do I lack adaptability?
A slipped disc is therefore not only triggered by external influences (overloading, incorrect loading, mishap, etc.). Psychological problems, such as mental overload, wrong mindset, etc., play at least as big a role in this context.
Possible psychological elements of disc complaints should therefore always be doubted – especially when standard treatment techniques do not lead to success.
If you would like to delve deeper into the subject of back pain and the subconscious, we recommend the following article: Back pain.
10. Anti-inflammatory measures against herniated discs.
If you suffer from inflammatory bowel disease, in addition to the recommendations already discussed, make sure you eat enough anti-inflammatory foods and/or supplements.
Foods with anti-inflammatory effects are sauerkraut, spinach, broccoli, fermented foods, onions, garlic, turmeric, ginger, cherries, blueberries, apples, etc.
Also use an anti-inflammatory omega3 oil such as hemp or linseed oil in cold cooking. Although these oils should not be heated, they can certainly be added over already prepared food.
Since magnesium has also been proven to have an anti-inflammatory effect, magnesium-rich foods such as amaranth, quinoa, millet, wild rice, pumpkin seeds, poppy seeds, sunflower seeds, almonds, chard, nettle, purslane, basil, marjoram and sage should not be missing from the diet.
The ideal dietary supplement for swellings of any kind is a combination of krill oil and astaxanthin. Both substances are effective antioxidants. They are able to render inflammation-promoting free radicals harmless and thus contain existing inflammatory processes.
11. Collagen-building substances against herniated discs
Glucosamine is a natural compound found in cartilage. Glucosamine supplements are made from glucosamine extracted from mussel shells or produced in a research laboratory. Research studies have shown that glucosamine can help improve cartilage material or slow its breakdown due to ageing or disease. This could help prevent or relieve neck and back pain.
In a healthy and balanced state, the intervertebral discs have a high collagen content, which contributes significantly to their stability and adaptability. In the course of the ageing process, however, this content decreases significantly. Therefore, you need to supply your overstressed intervertebral discs with collagen-forming substances that successfully support their regeneration and also help to prevent further herniated discs.
Among the most effective is a blend of high-dose natural silicon with glucosamine and chondroitin. This supplement is available in liquid form and is essentially unappetising. It can significantly support the strengthening of your intervertebral discs.
12. Nutritional components for spinal health
Omega-3 fats
Clinical research has shown that Omega-3 fatty acids can minimise inflammatory processes and disc degeneration in back pain. The 3 most important omega-3 fatty acids. ALA (alpha-linolenic acid) is the most important. The other 2 are DHA (docosahexaenoic acid) and EPA (eicosapentaenoic acid). The reason individuals need to consume a lot of vegetable oils and fish and shellfish is that ALA, EPA and also DHA are generally taken in through food, including supplements.
Vitamin D
Vitamin D is one of the most important vitamins for back health, as its function in bone and joint health and well-being is well documented. Research studies have shown that people who have undergone surgical treatment for degenerative spinal conditions have actually had significant vitamin D deficiency. Vitamin D is very important for the health of the bones and also the discs in the spine, which are made of collagen. It helps with calcium absorption. Taking vitamin D can additionally reduce back pain as it improves the health of the bones and cells in the spine.
Vitamin C
Another vitamin for spinal health and well-being is vitamin C. Vitamin C is important for healthy collagen formation, which makes up the spinal discs. It is also essential for the wellbeing of ligaments, tendons and bones. Vitamin C helps cells develop into healthy and balanced cells and serves as an antioxidant that prevents abnormal cell development. It also strengthens the body’s immune system. Vitamin C can relieve back pain if it is due to a spinal condition or prevent it by contributing to a healthy and balanced spine and healthy cells.
More information on herniated discs.
In addition to the presented natural measures for slipped discs, many other therapies and possibilities can be exhausted, even very simple things are welcome, the main thing is that they do good, calm and relieve the pain.
And please do not forget that a slipped disc always has a psychological component. Therefore, take some time and think about what particular concern might be behind your condition and what options are available.
If you feel that you are not getting anywhere on your own, ideally consult an experienced specialist to solve the problem in the mental area and ensure that your discs never have to point it out to you again.
FAQ
How exactly do I know if I have a herniated disc?
A herniated disc in the lumbar spine typically makes itself felt through very strong, stabbing back pain. These increase with movement, especially when the patient bends or lifts something. Coughing and sneezing can also increase the discomfort, which occasionally radiates to the buttocks or leg.
Does a slipped disc disappear again by itself?
For many people, a herniated disc heals on its own within six weeks. Until then, numerous treatments are offered to relieve the pain and improve mobility.
Where does the pain occur with a herniated disc?
Often the disc between the fourth and fifth vertebrae of the back or between the fifth lumbar vertebra and the coccyx is affected. The sciatic nerve also runs along this point. If the herniated disc presses on this nerve, the back pain often radiates into the buttocks or leg.
What should you refrain from doing in the event of a slipped disc?
Sports with distinct loading optima and those that involve strong rotations in combination with lateral dispositions – for example, golf, winter sports, video game sports and rebound sports such as tennis, badminton and squash.
How is the herniated disc repaired?
Only about 1 % of people with a herniated disc need surgical treatment today. Normally, a recovery time of about 12 weeks is expected. During this time, training and also private physiotherapy is an important part of the treatment of herniated discs.
Should you do sports with a slipped disc?
Over time, rest certainly does not help after a slipped disc, but normal training and also activity with the aim of stabilising the body, strengthening the muscles and relieving the strain on the discs. Everyday activities can also help.
Is cycling a good thing for the intervertebral disc?
Of course, cycling is good for you. … Stabilising the back muscles is a positive side effect that can be achieved by normal cycling, one to two hours a week, without additional special back training.
Are walks useful with a slipped disc?
Research suggests that regular walks or fast walking are also helpful for neck and back pain – for example, every other day for 30 to 60 minutes.
What helps better with a slipped disc: heat or cold?
When a pinched nerve triggers back pain, cold relieves the severe discomfort better. This is true, for example, in cases of sciatica, slipped discs or lumbago. In these problems, the surrounding tissue continues the nerve fibres and sends pain stimuli to the brain.
ICD codes for this disease: G55 | M50 | M51
ICD codes are internationally valid codes for medical diagnoses. They can be found, for example, in doctors’ letters or on certificates of incapacity for work.
The web content of ÁYIO-Q.com is for your information and in no case replaces a personal consultation or treatment by a qualified physician. The contents of ÁYIO-Q.com cannot and must not be used to make independent diagnoses or for self-medication.
Sources:
- NaPier Z, Kanim LEA, Arabi Y, et al. Omega-3 Fatty Acid Supplementation Reduces Intervertebral Disc Degeneration. Med Sci Monit. 2019;25:9531-9537. Published 2019 Dec 14. doi:10.12659/MSM.918649
- Zolfaghari F, Faridmoayer A, Soleymani B, Taji M, Mahabadi M. A Survey of Vitamin D Status in Patients with Degenerative Diseases of the Spine. Asian Spine J. 2016;10(5):834-842. doi:10.4184/asj.2016.10.5.834
- Dionne CE, Laurin D, Desrosiers T, et al. Serum vitamin C and spinal pain: a nationwide study. Pain. 2016;157(11):2527-2535. doi:10.1097/j.pain.0000000000000671
- Glucosamin, at https://www.mayoclinic.org/, accessed 15-12-2021















