Updated on 30. June 2022 from ÁYIO-Q Redaktion
Reading time: approx. 25 minutes
The common disease periodontitis: How you can save your teeth
Periodontitis – It is one of the most common chronic diseases worldwide. In Germany, about 11.5 million people suffer from a severe form of periodontitis. The disease usually begins insidiously and goes unnoticed by the person affected. If it remains untreated for a very long time, it can lead to tooth loosening and even tooth loss. Almost every second person suffers from more or less pronounced periodontitis in the course of his or her life.
However, periodontitis does not only threaten the teeth. Chronic periodontitis is also a risk factor for cardiovascular diseases and diabetes. Typical signs and symptoms of periodontitis are red to blue discoloured gum tissue and bleeding gums. Learn everything you need to know about the symptoms, causes and treatment of periodontitis here.
- Description
- Symptoms
- Shapes & Risk Factors
- Causes
- Diagnosis
- Progress & Forecast
- Conventional Medicine Treatment
- Preventive Measures
- Natural & Alternative Therapies
What is periodontitis?
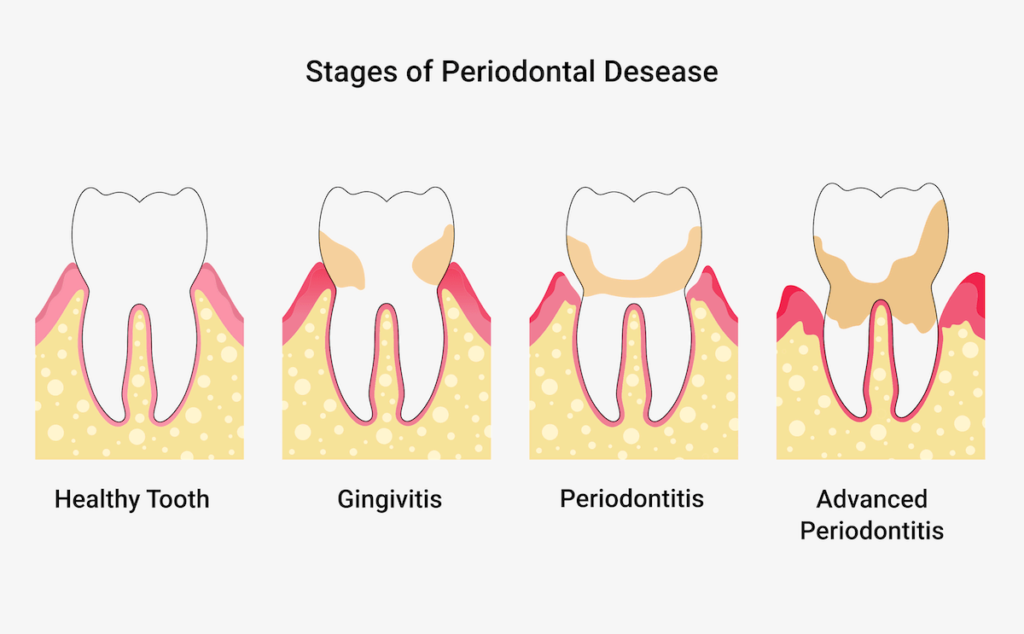
Periodontitis, often referred to as periodontosis, is a chronic bacterial inflammation of the periodontium and also of the gum tissue, which can lead to tooth loss. The periodontium, also called the “periodontium” (around the tooth), is made up of 4 different components: The gums, the tooth itself, the tooth socket and also the periodontium. If one of the parts of the periodontium is affected by this inflammation, it is called periodontitis and is expected to gradually affect the other parts of the periodontium.

In general, the term periodontal disease is typically used in the context of gingivitis. However, this is not the medically correct definition. Parodontosis, also called receding gums, is the primarily age-related and also inflammation-free loss of the tooth-supporting apparatus (= connective tissue), whereby the jaw bone (= bone substance) is frequently affected. Just as in the case of untreated periodontitis, teeth can fall out as a result.
Next to caries, gum diseases are the most common clinical picture in dentistry. After the age of 45, periodontitis is one of the main reasons for teeth falling out. However, according to research young people are also increasingly affected by periodontal disease. For example, about one in seven people under the age of 30 struggles with periodontitis.
This is a nuisance for everyone who brushes their teeth regularly and assumes that they are doing a lot right. But not all tooth cleaning is the same. In most cases, the brushing strategy must first be learned or trained on the patient’s own teeth as part of therapy-oriented oral prophylaxis. Furthermore, the risk of developing periodontitis varies from person to person.
In any case, it is clear that healthy and balanced, firm gums are an important protection against tooth loss and thus also against dentures.
What are the symptoms of periodontitis?

Common signs of the disease are bleeding gums and bad breath. If these changes occur more frequently, you should consult a dentist quickly. Other irregularities can also be considered symptoms of periodontitis:
- Bleeding gum tissue (e.g. during home oral hygiene and also spontaneously).
- Reddened, inflamed and also sensitive periodontium
- Gum recession (enlargement of the gum line or dark triangles between the teeth)
- Periodontal sites sensitive to touch
- Sensitive necks of teeth
- Incessant bad breath or a persistent undesirable taste in the mouth
- Pus discharge from the periodontal pockets
- Loose or protruding teeth (larger tooth spacing)
- Changes in chewing (bite)
- Altered prosthesis fit, poor hold of the prosthesis
- Gingivitis
If you notice several of these warning signs or symptoms, be sure to contact a dentist and share your observations. She or he can give you additional information or refer you to a specialist in periodontology.
What are the different forms of periodontitis?
In 1999, researchers established an international category of gum disease, which has also been proposed in Germany since 2001. According to this, periodontitis was classified as either persistent, aggressive, necrotising or a manifestation of a systemic disease. However, for some years now there has been a new classification which includes the following 3 types of periodontitis:
- Periodontitis
- Necrotising periodontitis
- Periodontitis as a manifestation of a systemic disease
Dangerous element: Necrotising periodontitis
Necrotising ulcerative periodontitis (NUP) is an unusual but particularly transmissible and fast-moving form of the disease. It is accompanied by marked bleeding of the gum tissue, tissue death, ulcers in the gum tissue between the teeth and also pain. In addition, there is bad breath, swollen lymph nodes and supposed pseudomembranes (form as a result of the inflammation from dead tissue cells and also have no orderly large tissue framework).
NUP is due to an infection with microorganisms that are also present in the oral cavity of healthy people, but have multiplied excessively in the affected patients. This often happens, for example, in HIV-infected people with their damaged endogenous immune system. Necrotising periodontitis is therefore sometimes also called HIV-associated periodontitis.
Necrotising ulcerative periodontitis (NUP) and also necrotising ulcerative gingivitis (NUG) are jointly called necrotising gum disease. They are different phases of one and the same infection: As long as only the gum tissue is affected, the dentist diagnoses NUG. If the inflammatory and also degrading processes have affected the jawbone and also the connective tissue between the original cementum and the bone (desmodont), he speaks of NUP.
Risk factor – Systemic disease
Sometimes periodontitis occurs as part of a systemic disease (underlying disease). It is not always easy to determine whether the disease is causing the periodontitis or rather contributing to the progression of “normal” periodontitis, which comes from plaque.
The following systemic diseases are thought to affect the inflammation of the periodontium and thus contribute significantly to the loss of the periodontium:
- genetic diseases such as Down’s syndrome, extreme neutropenia (lack of neutrophil granulocytes), Papillon-Lefèvre syndrome, Cohen’s syndrome, epidermolysis bullosa, Ehlers-Danlos syndrome, systemic lupus erythematosus, glycogen storage disease, etc.
- Acquired immunodeficiency states: acquired neutropenia, HIV
- Inflammatory diseases such as epidermolysis bullosa, inflammatory diseases of the digestive tract (e.g. Crohn’s disease, ulcerative colitis).
In addition, there are underlying diseases that can influence the course of periodontitis. These consist of:
- Diabetic diseases (Mellitus)
- Obesity (Adipositas)
- Weakening of the bones
- rheumatoid joint inflammation and also osteoarthritis
- Psychological tensions and anxieties
- Smoking (nicotine addiction)
What causes periodontitis?
Periodontitis usually begins insidiously with inflammation of the gums (gingivitis). The main cause is poor oral hygiene. Plaque forms on the teeth due to insufficient or incorrect cleaning, especially at the junction between the tooth and the gums. The plaque consists of food residues, saliva, germs and also their metabolic products.
So one of the most common causes of irritated gum tissue is microbial plaque. Dental plaque is a thin, initially hardly noticeable film that consists largely of bacteria. It is mainly found at the junction between the tooth and the gum and can feel fuzzy when touched with the tongue. The metabolic products of the microorganisms in plaque can cause the gums to swell and become inflamed. Plaque can be removed by proper brushing. This suggests that the risk of gingivitis and also periodontitis can be reduced by good dental hygiene.
Periodontal inflammation and periodontitis can also be promoted by other conditions, e.g:
- genetic predisposition
- smoking
- Metabolic diseases like diabetes
- mental tension
- Diseases of the immune system
- Hormone changes during pregnancy
In addition, some people are much more susceptible than others. Similarly, it is possible that certain medications cause excessive growth of the periodontium, which complicates oral health and also promotes gingivitis. This applies, for example, to medicines that suppress the body’s immune system (so-called immunosuppressants) or medicines used to treat vascular and heart diseases.
Medical diagnosis of periodontitis
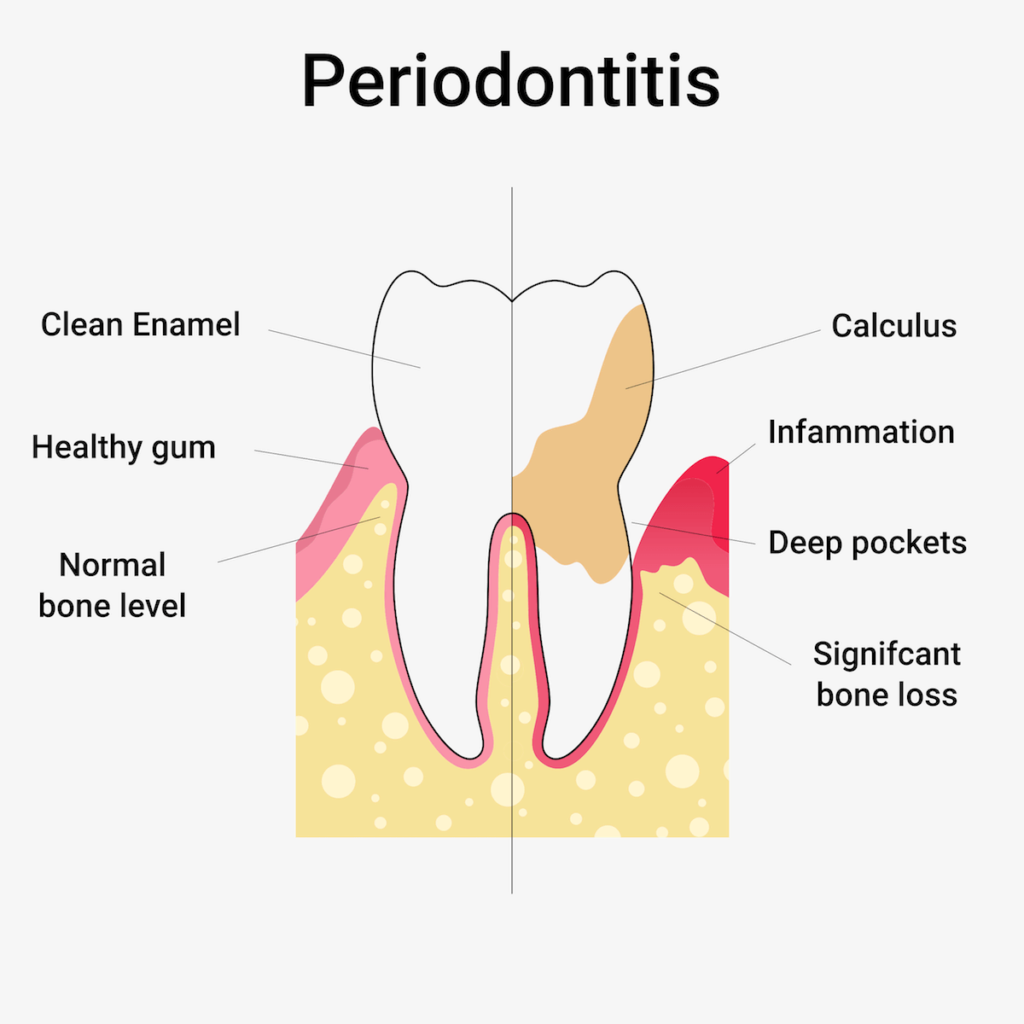
The dentist can detect periodontitis with the help of a tiny measuring probe: To do this, he measures the depth of the pocket on each individual tooth. He also determines the so-called blood index (PSI). This gives him a concrete overview of the condition of the teeth and also the extent of a possible inflammation.
With the help of a special probe, he carefully measures the depth of the individual gingival pockets and the bleeding tendency. He summarises the results in an index, the PSI (Periodontal Screening Index). There are 4 levels. At PSI 1 and 2, the pocket depth is less than 3.5 millimetres, but at PSI, tartar or plaque is already present and can become a danger. PSI 3 indicates mild to moderate periodontitis, and pocket depths are between 3.5 and 5.5 millimetres. PSI 4 means moderate to severe periodontitis with pocket centres of more than 5.5 millimetres.
Course & prognosis of periodontitis
The inflammation of the gums can decrease, but it can also persist, increase and become periodontitis.
If gingivitis persists, the pockets between the tooth and the gum can become several millimetres deep, in some cases even much more than 1 centimetre. Microorganisms accumulate in the gingival pockets that you can no longer reach with a toothbrush. Microbial deposits form at the origin as well as at the neck of the tooth, which can solidify and can be easily removed in the orthodontist’s office. Increased deposits of the gums are called concretions – in contrast to increased deposits above the gums, which are called tartar. The deeper a pocket is, the more the bacterial plaque advances towards the base of the tooth.
Bacteria and also tartar in the pockets can cause further inflammation. In periodontitis, this attacks the periodontium. As it progresses, the jawbone around the teeth is also attacked and broken down. This can affect parts of the tooth root. The teeth can become loose over time, making it difficult or uncomfortable to eat. After that, they can no longer be held in place and may even have to be removed.
Gum problems occur in episodes. This means that short phases in which cells are destroyed differ from longer phases in which the disease does not progress further or the cells additionally sometimes recover. Nevertheless, periodontitis does not heal by itself.
Traditional therapy: physiotherapy and medication
The most important goals of periodontal treatment are to preserve as many teeth as possible and to restore the diseased periodontium. To achieve this, the progression of the disease must first be stopped or at least slowed down. The treatment is usually carried out in 3 phases:
- First or hygiene phase ( phase 1 ) – plaque is removed in numerous prophylaxis sessions and the patient is educated about home dental hygiene and the connection between treatment, dietary habits and active prevention.
- Gum treatment ( phase 2 ) – The prerequisite for effective therapy is the removal of bacterial plaque and tartar in the gum pockets with curettes (hand instrument) and ultrasonic cleaning device, possibly under regional anaesthesia. This causes the elimination of inflammation in the periodontium and a decrease in the inflammatory deepened gingival pockets.
- Follow-up and maintenance treatment ( phase 3 ) – Checking the effectiveness of home dental care and, in particular, thorough professional cleaning of all bacterially contaminated tooth surfaces above and below the periodontium at regular intervals (2-6 times per year) as part of a therapy-oriented oral treatment programme.
It is equally important to realise that damage to the periodontium caused by periodontitis or periodontosis is not completely reparable. Therefore, prevention, early detection and also treatment are of high value.
How can I prevent periodontitis?
Mindful dental care with regular tooth cleaning plays a crucial role in optimal prevention.
No gingivitis without plaque
Generally speaking, without plaque or plaque in the mouth, there is no gingivitis and thus no chronic gingivitis. Without chronic gingivitis, periodontitis can almost be ruled out.
Consistent dental hygiene is the be-all and end-all
Daily, properly performed oral hygiene at home is the most important element of effective periodontitis treatment. It must also be clear that oral therapy alone is neither sufficient for prevention nor for permanent therapy. The dentist or dental hygienist can help prevent it by consistently removing tartar (hard plaque).
20 natural remedies against periodontitis and gingival atrophy
Brush up the oral flora
While the article on periodontitis above was more about classical therapy methods, you will now learn how periodontitis can be treated holistically with the help of alternative medicine. Gum disease often starts unnoticed with an inflammation of the gum tissue that spreads further and further. This can cause gum pockets to form and the teeth to lose their hold in the jaw. For this reason, it is important to detect this disease as early as possible and treat it accordingly. This is also possible with completely harmless treatments that strengthen your teeth and the periodontium without putting any strain on your body.
1. Milieu Therapy
Once the hygienic aspects are resolved, the other procedures can be taken to help. Complementary medicine treatment tries to maximise the milieu together with the approaches of standard medicine.
This is done with the following points:
- Strengthening the body’s immune system through phytotherapy and stress and anxiety control
- antibiotic foods and also herbs
- Harnessing the cleansing properties of raw foods
- Optimisation of the acid-base balance through nutrition
- Promotion of saliva formation
- Reduction of environmental pollution and luxury poisons
2. Oil Pulling For Periodontitis
Brushing teeth with water and toothpaste is now firmly integrated into everyday life. However, this does not eliminate all microorganisms, but only the water-soluble particles. But there are still fat-soluble fragments that continue to spread unhindered. You can get rid of these by oil pulling. Coconut oil or sesame oil are suitable because they are said to have an anti-inflammatory effect.
Take a teaspoon of the oil and drag it over the interdental spaces for about 5 minutes. After that, you can brush your teeth normally.
Perform an oil rinse (also called oil pulling) twice a day with a teaspoon of high-quality sesame or coconut oil, optionally also olive oil. On the one hand, the oil rinse has a massaging effect on the stressed tooth necks. On the other hand, it is able to draw the metabolic pollutants of the microorganisms out of the gum tissue.
Mouthwashes with anti-inflammatory properties, such as sage or rosemary, have proven effective during the day. You can use these both during periodontitis therapy and afterwards.
3. Astringents Against Blood Loss
Active substances such as tannins cause a closure of the surface by removing water from it. The mucous membranes feel really dry and also rough afterwards. This stops blood loss, and an antibacterial effect also complements the spectrum of action. The following astringents have proven to be effective:
- Tormentilla (Bloodroot)
- Ratanhia root
- Myrrh
Don’t forget: Tannins can be perceived as unpleasant if salivation is insufficient.
4. Strengthening The Immune System
Fighting the signs and symptoms is one point, fighting the cause is another. A solid, undamaged immune system also recognises and stops infections in the body – without outside help. This also has an effect on gingivitis and periodontitis.
Today’s modern diet hardly contains all the minerals, vitamins as well as various other nutrients that the body needs for a solid immune system. Important are:
Vitamins A, B, D, E, C and K2. As well as folic acid, magnesium, calcium and also omega-3 fatty acids. Renewing your vitamin stores is not only good for your immune system. Your saliva additionally mineralises and can thus pass these minerals on to your teeth and gums – strengthening them.
Antioxidants improve your protection against free radicals, which relieves your immune system. Antioxidants are found, for example, in fresh vegetables, fruit and also legumes. It is also important that you offer little food to the existing germs in your mouth. If you reduce your sugar consumption, the germs can be “starved out”.
5. Vitamin A In Periodontitis
Vitamin A, also called retinol, belongs to the fat-soluble vitamins and is mainly found in animal foods. Plant foods, on the other hand, may contain vitamin A precursors, which are called provitamin A or carotenoids.
Vitamin A ingested with food is stored in the liver, while ingested provitamin A is broken down in the small intestine and converted into other vitamins.
In our organism it is mainly needed for the following processes:
- the function of the body’s immune system – with a vitamin A deficiency, the number of infections increases
- the formation of new cells in the skin and also in the mucous membranes – a deficiency can lead to cell damage that heals only insufficiently; especially in the case of periodontitis, the supply of vitamin A can promote healing.
The daily requirement of a healthy and balanced adult is 0.8 to 1 mg of retinol, which is supplied as pure vitamin A or convertible provitamin A. You find vitamin A mainly in liver, fish, dairy products as well as eggs. Provitamin A is mainly found in green leafy vegetables as well as in red, yellow and orange vegetables and fruits – if these are prepared briefly, the body can absorb the carotenoids better.
The intake of food supplements is recommended for:
- Vegetarians and vegans who cannot cover their vitamin requirements through their diet
- Pregnant and breastfeeding women have an increased requirement
6. Vitamin C For Periodontitis
Vitamin C is also known as ascorbic acid. It can only be absorbed through food and cannot be stored in the body.
Vitamin C is essential for dental health, especially because of its role in:
- the body’s own immune system: if the vitamin supply is right, our body’s defences can properly deal with caries pathogens and other pathogens. If the body lacks vitamin C, both the protection against inflammation and the healing of injuries are impaired.
- the formation of connective tissue cells, teeth, gum tissue and bones: The best-known vitamin C deficiency disease, scurvy, used to affect seafarers in particular and was initially manifested by bleeding tooth necks and teeth falling out.
The guideline value for healthy adults is 95 or 110 mg of vitamin C per day (especially for women and men). Vitamin C is mainly contained in fresh vegetables and fruit, but is very quickly degraded on contact with light, heat and oxygen, so that freshness and raw consumption or the shortest possible cooking time are particularly important here. Additional vitamin C supplements are usually not necessary in a balanced diet, exceptions are:
- Older people with an extremely unbalanced diet plan
- Cigarette smokers with a very one-sided diet plan
7. Vitamin B12 In Periodontitis
When it comes to oral health, vitamin B stands not only for what we would like to see, namely a good connection with your dentist, but above all for vitamin B12, also called cobalamin.
Vitamin B12 is mostly absorbed through animal foods and can be stored in the liver. Signs and symptoms of a deficiency therefore only become noticeable in the case of a permanent undersupply.
A deficiency of vitamin B12 can lead to anaemia and is also often manifested by sores on the mucous membranes of the mouth. Our body generally needs vitamin B12 for:
- the formation of red blood cells
- the formation of new DNA during cell development
- the absorption of folic acid
A healthy and balanced adult consumes about 3 µg of vitamin B12 daily. The majority of this vitamin is found in animal foods such as meat, fish, eggs and milk – as little as 100 g of Emmental cheese or 60 g of minced meat is enough to cover the daily requirement.
Food supplements are particularly recommended for:
- Vegans who cannot sufficiently cover their vitamin needs with plant foods.
- People who suffer from diseases of the stomach, intestinal tract or pancreas, or who take medication that impairs vitamin B absorption.
8. Vitamin D In Periodontitis
The vitamin D3 (“calcitriol”) is a hormone that plays a crucial role in bone formation and has the ability to minimise inflammation.
Patients with high vitamin D3 levels have less bleeding gums and less pocket depth. Early tooth loss can thus be prevented. Furthermore, vitamin D3 has both immunological and metabolic effects on our body. Autoimmune diseases, joint inflammation and also diabetes mellitus occur particularly frequently with low D3 levels.
Since vitamin D3 supports the body’s immune system, a deficiency can have the following consequences:
- Cardiovascular problems and cardiac arrest
- States of concentration and also rest
- Malaise
- depression
Diseases such as bronchial asthma and cancer are also associated with reduced D3 levels. Adequate vitamin D3 levels have been found to confer resistance to influenza. Studies show that patients with 25-OH vitamin D3 (calcidiol) levels above 80ng/ml are 85% protected against many chronic diseases.
They are usually recommended for weakening bones, but they can also have a positive effect on the immune system and jaw bones, as several recent researches show.
9. Vitamin K In Periodontitis
Vitamin K is divided into vitamin K1, the so-called phylloquinone, which is ingested with food, and vitamin K2, the so-called menaquinone, which is produced in the body by intestinal bacteria.
Our body needs vitamin K mainly for the:
- Bone formation: Here vitamin K works in conjunction with vitamin D as well as calcium to maintain the stability of the bone tissue. This is important for the well-being of the teeth, because only a stable jawbone gives the teeth support.
- Blood clotting: With a vitamin K deficiency, bleeding occurs much more frequently. The oral mucosa and also the periodontium are also affected.
Healthy adults need 60 to 70 g of vitamin K daily (especially women and men), with the need increasing from the age of 50.
Vitamin K is mainly found in green leafy vegetables, cabbage and poultry meat. A vitamin K deficiency is relatively rare; supplementary preparations are recommended by doctors especially for the following groups of people:
- Newborns and infants in the breastfeeding phase
- Osteoporosis patients
- People with certain diseases, e.g. Crohn’s disease, coeliac disease, and people who need to take certain medicines, e.g. prescription antibiotics, phenobarbital.
- People with alcohol-related liver damage that causes vitamin K deficiency
10. Minerals For Periodontitis
Not only vitamins, but also minerals are very important for keeping the teeth and the periodontium healthy. Calcium and fluoride are the most important.
Calcium (also called calcium) is an important basis of our bone cells.
Calcium is important for dental health and well-being for 2 reasons:
- It promotes the remineralisation of teeth and makes them resistant to degeneration
- It ensures the safety of the jawbone and thus also the stability of the teeth resting in it
2. phosphorus Or Phosphate Is Another Major Component Of Dentin And Tooth Enamel. Again, Vitamin D Is Needed To Store The Dietary Phosphorus In The Bones And Teeth.
3. Fluorides Increase Resistance To Caries And Thus Protect Against “holes” In The Tooth. The Setting Of The Activity Is Twofold:
- They strengthen the enamel and make it particularly resistant to acids.
- They reduce the metabolism of caries bacteria and thus prevent them from multiplying.
They strengthen the enamel and make it particularly resistant to acids.
They reduce the metabolism of caries bacteria and thus prevent them from multiplying.
4. magnesium – In Recent studies magnesium Is Even Thought To Have An Anti-inflammatory Effect. Thus, Fewer Cases Of Gingivitis And Periodontitis Are Observed With A Sufficient Magnesium Supply.
11. Omega-3 Fatty Acids In Periodontitis
Researchers from Harvard University and the Harvard Institution of Public Health Israel Deaconess Medical Facility, after extensive research studies, found that the higher the consumption of omega-3 fatty acids, the lower the rate of periodontal disease in the United States population.
In addition, therapy of the gum problem with high-quality omega-3 fatty acids would also be helpful for various other chronic inflammatory diseases such as asthma, inflammatory bowel disease, arthritis and so on.
Integrate oils rich in omega-3 fatty acids into your diet, such as linseed oil, hemp oil or krill oil, /a> for example. Subsequently, 1 to 3 tablespoons daily or, in the case of krill oil, the indicated amount of capsules is currently sufficient.
12. Tea Tree Oil
Due to its solid antiseptic effect, tea tree oil is excellent for fighting bacteria and inflammation in the mouth. The easiest way is to use a toothpaste with tea tree oil. In addition, you can apply a few drops of tea tree oil to your interdental spaces several times a day.
13. Turmeric
Turmeric has a whole range of beneficial properties. If you have problems with your gums, you can make a paste of 1 teaspoon of turmeric extract, 1 teaspoon of crystal salt and half a teaspoon of mustard oil and use it twice a day.
14. Sage And Also Thyme
A mouthwash made from natural medicinal herbs such as thyme and sage can quickly provide significant relief from periodontal disease. Simply add 2 tablespoons of sage or thyme to a cup of warm water. After 15 minutes of soaking, you can use your natural mouthwash. We recommend using and consuming the mouthwash throughout the day.
15. Burdock Root
A burdock root mouthwash is also excellent for combating periodontal disease. Simply add a teaspoon of burdock root to a cup of warm water and strain after half an hour. The mouthwash prepared in this way must be used extensively several times a day to rinse the mouth.
16. Clove Oil
Another natural home remedy that is popular for bleeding or sore tooth roots is clove oil. Again, a little clove oil is applied daily to the periodontal areas with a finger.
17. Green Tea
According to research, green tea can stop gum recession naturally. Therefore, 2 glasses of green tea per day must be enough to proactively serve their own dental hygiene.
18. Aloe Vera
The application of aloe vera can lead to a significant improvement in existing gum inflammation due to its antibacterial properties. It is best to apply aloe vera gel to the affected areas several times a day.
19. Baking Soda (Baking Powder)
One of the best-known natural remedies for gingivitis is baking soda. It is really easy to use: Simply mix a paste of bicarbonate of soda and a little water in the morning and evening and apply it to the gums with your finger. After 10 minutes, rinse your mouth thoroughly and brush your teeth as usual. Or you can brush your teeth with it right away.
20. Strengthen Self-healing Powers In Periodontitis
Various studies show the connection between periodontitis and vascular diseases (such as arteriosclerosis) or diabetes. The question of interest must therefore be how to support patients with such inflammatory gum disease, which can lead to tooth loss.
One focus of Brazilian scientists responsible for their study is on supporting the self-healing powers of sufferers. The theory underlying the study is that a holistic therapy that goes hand in hand with the typical gum treatment can restore the patient’s vitality and stop the dynamic process of inflammation-induced bone loss in the jaw area.
A total of 60 people took part in the study: 40 were struggling with chronic periodontitis, while another 20 people, who served as the control group, had no problems in this regard. All periodontitis clients received standard treatment as part of the usual periodontitis therapy (education, individual dental hygiene advice, measurements of the tooth pockets). Fifty percent of these patients additionally received a holistic treatment according to the Similé principles.This consisted of a laxative solution (Berberis in potency C 6, 2 times 2 tablets daily), an intensive cure (Mercurius solubilis, Belladonna or Hepar sulphuris, in potency C 6, three times 2 tablets daily) as well as the nosode Pyrogenium to promote energy balance (in potency C 200, one dose weekly). At the beginning and also at the end of the research study after 90 days, not only were medical criteria for periodontitis collected, but also serological analyses were carried out to determine cholesterol, triglyceride, sugar and uric acid levels.
For the professional criteria such as probing depth, plaque index and also the degree of gingival bleeding, a significant improvement was achieved in both treatment groups. On the level of serological values, the additional therapy with holistic treatments was superior to the typical therapy.
Finally: Can damaged and dead teeth make the whole body sick?
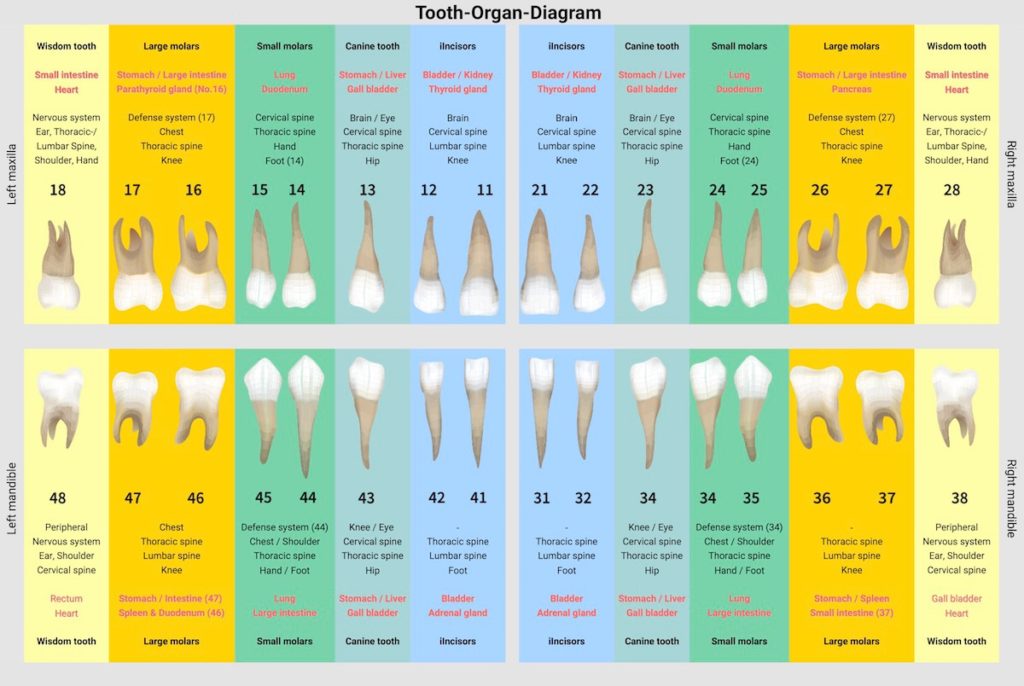
A centuries-old quotation by Paracelsus has lost none of its relevance to this day: “A whole person hangs on every tooth.” The importance of human teeth goes far beyond the function of chewing. Dental diseases are not only a purely aesthetic problem, they mean much more pain, damage and far-reaching consequences for the entire body. Teeth, organism and psyche are closely connected, influence each other and can be the cause of a whole range of chronic diseases. Thus, a diseased tooth can easily weaken the whole body and a disturbed jaw joint can lead to back, head and neck pain as well as ringing in the ears. Behind every tooth is an organ. If a tooth is ill, this can become noticeable in the corresponding organ and vice versa. To get rid of the complaints in the long run, the cause must be determined so that both interference fields, teeth and organism, can be treated.
It has long been assumed in naturopathy that each tooth has a relationship to a certain organ. Especially in traditional Chinese medicine, this principle has been valid for 4000 years. Signals that our body sends us can be read from the teeth. Conversely, a diseased organ can damage the corresponding tooth.
The health of the teeth is an expression of a healthy organism.
FAQs
How dangerous is periodontitis?
The risk of periodontitis is often ignored by those affected. If left untreated, periodontitis not only leads to missing teeth and thus expensive dentures such as implants. No, it can also lead to major substantial damage throughout the body. Depending on pre-existing underlying problems such as diabetes, there is an increased risk of retinal or kidney damage. The risk of cardiovascular disease or strokes can also increase.
Is periodontitis treatable?
Periodontitis is a stubborn disease that can be stopped, and in some circumstances completely cured. With the right treatment, the progression of the disease can be stopped and the associated tooth loss can also be prevented. Patients suffering from chronic gingivitis require long-term treatment.
Is periodontitis contagious?
Periodontitis is triggered by bacteria. This means that periodontitis is actually a communicable disease and, above all, contagious. At the same time, transmission through coughing in the form of a pearl infection is extremely unlikely. Transmission is most likely through the use of the same toothbrush or through direct contact such as extensive kissing. If you have acute periodontitis, make sure that other oral care items such as interdental brushes and toothbrush cups, as well as glasses and cutlery, are only used by one person. Another recommendation is to consider the life partner, if necessary, as well as the offspring during periodontal treatment, even if the partner or the child does not programme any signs.
Which bacteria cause periodontitis?
Microbial strains that are capable of triggering periodontitis are also called periodontitis marker germs or lead germs. If these bacterial loads are present in appropriate numbers, periodontitis is likely.
The identification of these bacteria plays an essential role for targeted antibiotic periodontitis treatment, among other things. A microbial test is used to search for the following marker germs:
- Porphyromonas gingivalis (P.g.)
- Tannerella forsythia (T.f.)
- Treponema denticola (T.d.)
- Aggregatibacter actinomycetemcomitans (A.a.)
- Prevotella intermedia (P.i.)
Periodontal disease/periodontitis – What is the difference?
In common usage, the terms periodontitis and periodontosis are often used synonymously. Periodontal disease is associated with aesthetic factors and additionally with increased sensitivity due to exposed tooth necks. The suffix “-itis” in periodontitis, on the other hand, indicates that it is a chronic microbial infection of the periodontium and gum tissue that can lead to tooth loss.
Can I have periodontitis even if my gum tissue is not bleeding?
Yes. Periodontitis is usually chronic and painless. Usually, the inflammation occurs in the periodontal pockets that have developed. Even if you brush your teeth, the gums do not bleed all the time.
Is periodontitis genetic?
A study from 2017 suggests that the risk of periodontitis can be inherited. In the world’s largest study of genetics and periodontitis, a team of researchers from Berlin’s Charité University Hospital found that the risk for the stubborn swelling of the tooth bed is also hereditary. Further studies are to follow.
Why is periodontitis called a “silent” disease?
A crucial background is that a chronically inflamed periodontal pocket is recognisable by occasional blood loss from the gums, but not by discomfort. This type of inflammation is also described as being directed inwards and therefore usually remains invisible from the outside. And even that which is not detected and does not cause severe pain simply goes unnoticed. In order not to be at the mercy of this fate, a self-check and a periodontal basic examination (PGU) by a dentist with special training in periodontology can help.
What is apical periodontitis?
This form of periodontitis is also called root tip inflammation. In such a case, there is a bacterial infection at the tip of the tooth root. Elimination of the infection by root canal treatment is appropriate. There may be sudden very severe discomfort or wear and tear of the jawbone, even tooth loss. The bacteria can also enter the bloodstream and cause inflammation in various other parts of the body.
Is periodontitis associated with pain?
Depending on the stage of development, form and area, periodontitis can be completely painless for a long period of time. Therefore, periodontitis is usually not recognised or neglected. The symptoms do not take the form of the usual toothache as with caries. Rather, there is increased severe blood loss, inflammation and also pain of the gums. If these warning signs are overlooked, there is an increased recession of the periodontium as well as the teeth becoming particularly sensitive due to the exposed neck of the tooth and thus also much more susceptible to complaints.
How exactly do germs get from the mouth into the rest of the body?
Our teeth are connected to the body via nerves and capillaries. If a tooth root is inflamed, toxic substances from microorganisms can enter the bloodstream via the tooth root tip and attack our body organs. Especially when immune protection is weakened, which is typically the case with infants, the elderly or sick people, unwanted invaders from the mouth have an easy time.
ICD codes for this disease: K05 | K05.2 | K05.3
ICD codes are internationally valid codes for medical diagnoses. They can be found, for example, in doctors’ letters or on certificates of incapacity for work.
The web content of ÁYIO-Q.com is for your information and in no case replaces a personal consultation or treatment by a qualified physician. The contents of ÁYIO-Q.com cannot and must not be used to make independent diagnoses or for self-medication.
Sources:
- Sara Thorbert-Mros,Björn Kassel,Tord Berglundh, Age of onset of disease in subjects with severe periodontitis: A 9- to 34-year retrospective study, https://doi.org/10.1111/jcpe.12757
- Parodontidis – Klinischer Leitfaden, EFP – New klassification, European Federation of Periodontology, Published March 2019, accessed 22.01.2022
- Pihlstrom BL, Michalowicz BS, Johnson NW. Periodontal diseases. Lancet. 2005;366(9499):1809-1820. doi:10.1016/S0140-6736(05)67728-8
- Torpy JM, Burke AE, Glass RM. Periodontal Disease. JAMA 2008; 299(5): 598., accessed 20.01.2022
- Lang, N.P. & Tonetti, M.S.: Periodontal Risk Assessment (PRA) for Patients in Supportive Periodontal Therapy (SPT) in: Oral Health & Preventive Dentistry 1/2003, S.7-16
- Heidemann, D. (ed.): Parodontologie, Elsevier / Urban & Fischer Verlag, 4th edition, 2005.
- Hellwig, E. et al.: Einführung in die Zahnerhaltung, Deutscher Zahnärzte Verlag, 7th edition, 2018
- Martinon P, Fraticelli L, Giboreau A, Dussart C, Bourgeois D, Carrouel F. Nutrition as a Key Modifiable Factor for Periodontitis and Main Chronic Diseases. J Clin Med. 2021;10(2):197. Published 2021 Jan 7. doi:10.3390/jcm10020197
- Neiva RF, Al-Shammari K, Nociti FH Jr, Soehren S, Wang HL. Effects of vitamin-B complex supplementation on periodontal wound healing. J Periodontol. 2005;76(7):1084-1091. doi:10.1902/jop.2005.76.7.1084
- Fageeh HN, Fageeh HI, Prabhu A, Bhandi S, Khan S, Patil S. Efficacy of vitamin C supplementation as an adjunct in the non-surgical management of periodontitis: a systematic review. Syst Rev. 2021;10(1):5. Published 2021 Jan 4. doi:10.1186/s13643-020-01554-9
- Garg P, Ghalaut P, Dahiya K, Ravi R, Sharma A, Wakure P. Comparative evaluation of crestal bone level in patients having low level of Vitamin D treated with dental implant with or without Vitamin D3 supplements. Natl J Maxillofac Surg. 2020;11(2):199-206. doi:10.4103/njms.NJMS_49_20
- Reginster JY. The high prevalence of inadequate serum vitamin D levels and implications for bone health. Curr Med Res Opin. 2005;21(4):579-586. doi:10.1185/030079905X41435
- Uwitonze AM, Rahman S, Ojeh N, et al. Oral manifestations of magnesium and vitamin D inadequacy. J Steroid Biochem Mol Biol. 2020;200:105636. doi:10.1016/j.jsbmb.2020.105636
- Meisel P, Schwahn C, Luedemann J, John U, Kroemer HK, Kocher T. Magnesium deficiency is associated with periodontal disease. J Dent Res. 2005;84(10):937-941. doi:10.1177/154405910508401012
- Huang CB, Ebersole JL. A novel bioactivity of omega-3 polyunsaturated fatty acids and their ester derivatives. Mol Oral Microbiol. 2010;25(1):75-80. doi:10.1111/j.2041-1014.2009.00553.x
- Chatterjee A, Saluja M, Agarwal G, Alam M. Green tea: A boon for periodontal and general health. J Indian Soc Periodontol. 2012;16(2):161-167. doi:10.4103/0972-124X.99256
- Mourão LC, Moutinho H, Canabarro A. Additional benefits of homeopathy in the treatment of chronic periodontitis: a randomized clinical trial. Complement Ther Clin Pract. 2013;19(4):246-250. doi:10.1016/j.ctcp.2013.05.002
- Munz M, Willenborg C, Richter GM, et al. A genome-wide association study identifies nucleotide variants at SIGLEC5 and DEFA1A3 as risk loci for periodontitis [published correction appears in Hum Mol Genet. 2018 Mar 1;27(5):941-942]. Hum Mol Genet. 2017;26(13):2577-2588. doi:10.1093/hmg/ddx151
- da Silva MK, de Carvalho ACG, Alves EHP, da Silva FRP, Pessoa LDS, Vasconcelos DFP. Genetic Factors and the Risk of Periodontitis Development: Findings from a Systematic Review Composed of 13 Studies of Meta-Analysis with 71,531 Participants. Int J Dent. 2017;2017:1914073. doi:10.1155/2017/1914073