Updated on 8. December 2021 from Marc Hedemann
Reading time: approx. 15 minutes
Causes and therapeutic approaches.
Worldwide, the incidence of psoriasis ranges from 0.09 (Tanzania) to 11.4 percent (Norway). Thus, the chronic inflammatory skin disease is a serious global health problem affecting more than 100 million people.
Who treats psoriasis and is psoriasis curable? What can you do about it yourself? You can find answers to questions like these in the following article.
What is psoriasis actually?
The term psoriasis (psoriasis vulgaris, plaque psoriasis) is used by doctors to describe an inflammatory autoimmune disease of the skin. Although it can develop at any age, the disease usually breaks out before the age of 30 or around the age of 50. The predisposition is often passed on from parents to children. In the course of their lives, about two percent of men and women develop psoriasis.
Dandruff: Where does it occur?
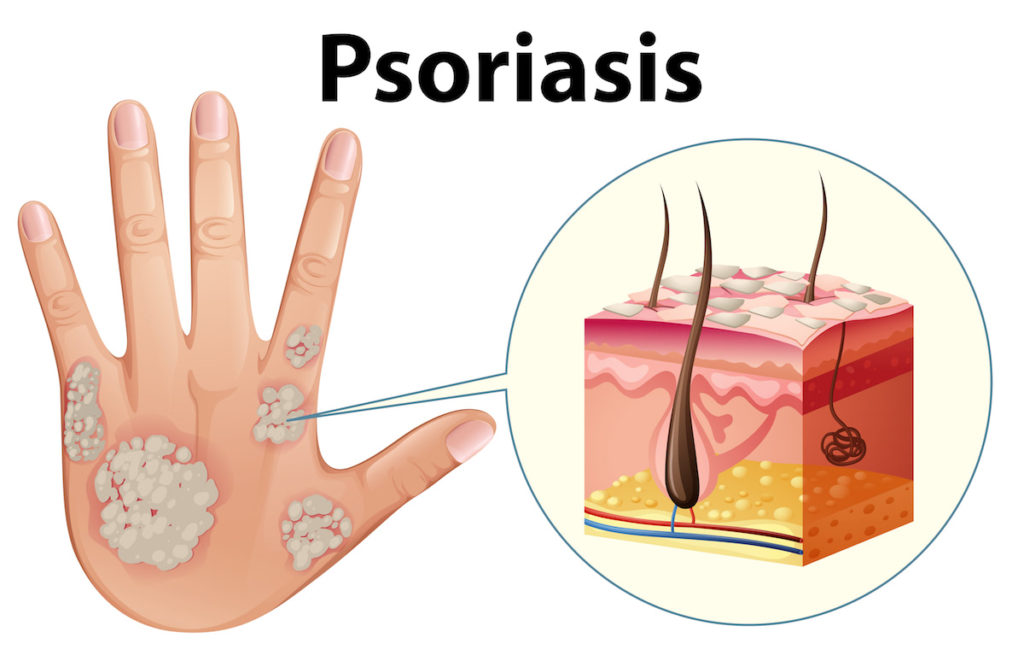
Typically, the disease manifests itself as dot-shaped to palm-sized, sharply demarcated red skin patches that are covered with silvery-white scales and trigger intense itching in attacks.

As a rule, the skin symptoms form
- on the outer sides of the large joints (elbow, knee and shin),
- the lower back (sacrum, buttocks, genital area),
- the hands and scalp.
The fingernails are often involved, turning yellow to brownish (nail psoriasis).1,2
Psoriasis has many faces.
Psoriasis manifests itself in different forms. Or to put it another way: every person affected has their own characteristic clinical picture. For this reason, psoriasis is often difficult to diagnose. Medicine knows many other causes for itchy and scaly eczema.
Classification of psoriasis
Depending on the age at which the disease typically manifests itself clinically, a distinction is made between the following 2 classes:
| Psoriasis type I (early form) | Psoriasis type II (late form) | |
|---|---|---|
| Age of manifestation | Between 10 and 30 years | Between 40 and 60 years |
| Frequency Type I vs. Type II | 60–70% | 30–40% |
| Genetic disposition | Familial cluster | Familial cluster rare |
| Clinical course | Often severe course | As a rule, milder course |
Dandruff – what types are there?
Doctors distinguish between different courses and manifestations. These include, among others:
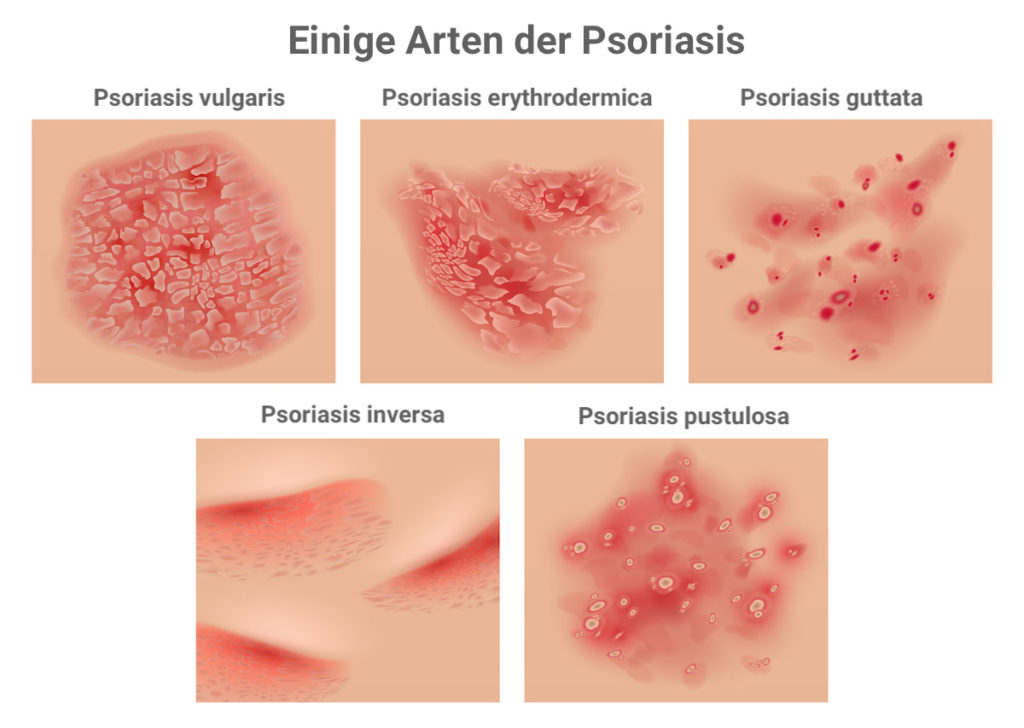
1. Inverse Psoriasis
In “reverse” psoriasis, the skin symptoms are not found on the outside (extensor sides) but in the backs of the knees and bends of the elbows.
2. Psoriasis punctata
The foci have a diameter of three to ten millimetres and mostly appear on the trunk of the body.
3. Psoriasis palmaris et plantaris
As the name suggests, eczema is limited to the palms of the hands and soles of the feet.
4. Psoriasis geographica
In this form of progression, psoriasis foci occur over a large area and have a map-like appearance.
5. Pustular psoriasis
This name comes from the fact that purulent pustules form on the skin manifestations. Five percent of people with psoriasis suffer from pustular psoriasis.
Is psoriasis contagious?
Psoriasis sufferers attract attention in the swimming pool or sauna. Because many people are afraid of infection. Did you know that lifeguards in Germany were allowed to remove people with psoriasis from swimming pools until 2005? Although thanks to the intervention of the German Psoriasis Association (DPB), the bathing regulations were changed, even today those affected are often ostracised.3
Since psoriasis is not an infectious disease caused by pathogens (bacteria, viruses, fungi), there can also be no transmission from person to person. Therefore, no one needs to shy away from close physical contact.
Dandruff – when to see a doctor?
When a red, scaly rash first appears, many people wonder: Is this psoriasis? If such symptoms are observed and the disease has already been diagnosed in another family member, the suspicion is obvious. A visit to a dermatologist provides certainty.
If the disease lasts ten years or more, organs can also be affected. Many sufferers call these late effects psoriasis that goes inside. In one in five patients, psoriasis spreads from the skin to the joints (psoriatic arthritis), leading to inflammation, swelling and pain.4
Psoriasis – possible concomitant diseases.
Psoriasis patients have an increased risk of so-called comorbidity. Doctors use this term to describe the phenomenon that one or more other diseases occur at the same time as the underlying disease. These include diabetes mellitus type 2, obesity, lipid disorders and cardiovascular diseases such as hypertension, atherosclerosis (hardening of the arteries), stroke and heart attack.5
Causes of psoriasis.
Who gets psoriasis? In orthodox medicine, the cause of the disease is considered to be an interaction of two different factors: an altered genetic make-up and certain triggers. Only when both are present does the disease break out. The change in the genetic material affects the human leukocyte antigen HLA-B27, which our body translates into a certain protein (gene expression).
HLA antigens (tissue compatibility antigens) play an important role in differentiating between the body’s own and foreign structures. They are found on all cells and signal to the immune system: I belong to you, don’t attack me.
In other words, psoriasis involves the translation of a defective HLA-B27 antigen into a defective protein, which in turn is incorporated into the cell surface of skin cells. The born immune system mistakenly thinks these proteins are foreign to the body and triggers an inflammatory response. Due to the inflammation, the skin-forming cells (keratinocytes) divide more quickly and reject unkeratinised skin cells in the form of silvery-white scales.
When does psoriasis break out?

Possible triggers of a psoriasis flare-up include:
- Mechanical factors such as tight clothing, scratching
- Infections (common cold)
- Hormonal changes (puberty, menopause)
- chronic diseases (Hashimoto’s thyroiditis, cancer)
- Medication (antibiotics, ACE inhibitors, beta blockers)
- Excessive stress, sunburn
The episodes, which last several days to weeks, are repeatedly interrupted by symptom-free intervals.
Overweight and obesity play an important role in psoriasis.
People who suffer from psoriasis often weigh too many kilos. With the abdominal girth (visceral fat tissue), the body’s tendency to inflammation also increases. According to private lecturer Dr. Sascha Gerdes from the Psoriasis Centre Kiel, obesity acts as a trigger factor for psoriasis. As a logical consequence, those affected should reduce their overweight.6,7
This recommendation by Dr Gerdes is based on several scientific research studies. A study by Italian scientists with 303 participants from 2014 came to the following conclusion: “The consistent change in diet in combination with physical exercise for 20 weeks reduced the severity of psoriasis in overweight and obese patients.”8.
As research results from 2020 show, a 12% weight loss is already enough to significantly reduce skin symptoms and itching.9.
Treatment of psoriasis with conventional medicine.

Depending on the severity of psoriasis, doctors use different strategies. UV radiation (PUVA), topical ointments and medications have one thing in common: they only treat the symptoms of the disease, as no causative treatment is available. Cortisone and cytostatics such as ciclosporin and methotrexate have significant effects on the immune system when used for a long time. Quite a few patients are therefore looking for alternatives.
In the meantime, conventional medicine offers a wide range of different active substances. These include so-called PDE-4 inhibitors and genetically engineered biologics. With drugs like adalimumab and infliximab, doctors also commonly prescribe monoclonal antibodies. These block pro-inflammatory cytokines and thus interfere with the body’s immune response.
Naturopathic treatments for psoriasis
Naturopaths and alternative practitioners also primarily try to alleviate the complaints of their patients and to prolong the symptom-free intervals. Among others, the following therapies have proven successful:
- Anti-inflammatory diet (Mediterranean diet) with a high proportion of vegetables, fruit, nuts and seeds (linseed, chia seeds)
- Homeopathic or herbal ointments and fat creams
- Washes with horsetail, sarsaparilla and quillaja bark
- Soybean oil or peanut oil with wheat bran extracts and whey for full baths
- Rubbing the affected areas with linseed oil
- Frankincense and evening primrose oil as food supplements
- Therapeutic fasting followed by the use of live intestinal bacteria (probiotics)
- If needed, add missing nutrients such as vitamin A, vitamin D, vitamin E, omega-3 fatty acids, zinc, selenium and coenzyme Q10.
- Stress reduction through autogenic training
- Autogenous urine therapy
In addition, it is important to drink enough high-quality water every day and not neglect detoxification (liver cleansing) and deacidification of the body.
As part of its globally respected health programmes, the ÁYIO-Q Centre of Vitality imparts valuable knowledge to promote mental and physical health. In addition to revitalising the skin, ÁYIO-Q offers, among other things, drinking water therapy with energised water. In a recent survey, 88 percent of the participants rated their physical and mental condition as better than before after 3 months of use.
Do vitamins, minerals and omega-3 fatty acids improve the symptoms of psoriasis?
Oxidative stress contributes to the development of psoriasis.
Many naturopathic doctors and therapists have long been convinced that oxidative stress plays an important role in the development of psoriasis. Current scientific research results actually point to a possible connection.10-12
But what exactly do scientists understand by the term oxidative stress? Simply put, it is extremely reactive oxygen compounds, so-called free radicals. They take on important tasks in energy production in the body (citric acid cycle) and support the immune system in fighting pathogens.13
However, these useful helpers have a dark side. When too many free radicals occur due to environmental influences and the body’s own processes, they destroy vital cell structures. Normally, our organism has sufficient amounts of antioxidants that immediately neutralise these dangerous oxygen compounds.
The most important antioxidants for us include vitamin E, vitamin C, selenium and zinc. However, the trace elements zinc and selenium only have an antioxidant effect when they are incorporated into the body’s own enzymes. Several scientific studies show that the concentrations of vitamin E, selenium and zinc in the blood are significantly reduced in people with psoriasis.14,15
What does this mean? The deficit of vital antioxidants proven in several studies indicates oxidative stress.

In 2008, a Russian research group conducted a study with a total of 58 psoriasis patients who were hospitalised. Half of the participants received a preparation with 50 mg vitamin E, 50 mg coenzyme Q10 and 48 mg selenium (antioxidant group) for 30 to 35 days.
The remaining subjects were administered an identical-looking agent without active ingredient (placebo group). The result: At the end of the study, the markers for oxidative stress in the antioxidant group had normalised. In addition, supplementation with vitamin E, selenium and coenzyme Q10 caused a significant improvement in the symptoms.16
Vitamin D and its role in psoriasis.
Since our body makes vitamin D in the outer layer of the skin, it is reasonable to assume that skin diseases such as psoriasis lead to a disruption in the body’s own production. Indeed, those affected have low levels of vitamin D in their blood.17

A deficiency of this important micronutrient is not uncommon in our latitudes. In patients with psoriasis, however, a vitamin D deficiency has negative effects on the further development of the disease. This is because vitamin D plays an important role in the proliferation (increase) and maturation of skin-forming cells (keratinocytes). For this reason alone, you should eliminate an undersupply immediately.
In addition, vitamin D has a proven effect when applied externally to the affected skin areas. Whether a long-term intake of the valuable micronutrient also leads to an improvement of the symptoms and a reduction in the frequency of the relapses is controversial. This is because no clinical study has yet determined the optimal daily dose of vitamin D for psoriasis patients.18
Diet has a significant influence on the course of psoriasis.
Like most chronic inflammatory diseases, the symptoms and course of psoriasis can be influenced by choosing the right foods. Anti-inflammatory nutrients is the magic word. As numerous scientific studies have shown, a Mediterranean diet has a positive effect on the symptoms as well as the severity of psoriasis.19-24
Our typical western diet ( Western pattern diet) consists of a high proportion of meat, processed animal products (sausage, ham, cheese) as well as bread, rolls and pasta made from white flour. These foods favour the development of inflammation in the body. The Mediterranean diet, on the other hand, is characterised by lots of fresh fruit and vegetables, olive oil, fish and seafood.

Cold-water fish such as mackerel, salmon, Baltic herring and sardines contain greater amounts of anti-inflammatory Omega-3 fatty acids. Recent studies suggest that the omega-3 fatty acids docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA) in particular are responsible for the beneficial effects of the Mediterranean diet.25,26
Basil, ginger, cumin, aniseed, fennel, turmeric, red pepper, garlic and rosemary are also excellent for people with psoriasis. In a recent research paper, scientists from Taiwan were able to show: Essential oils from fennel and cumin effectively counteract inflammation. For this reason, the authors recommend using cumin and fennel oil in the treatment of psoriasis.27
It is best to avoid fast food and other highly processed foods, sugary drinks and irritants such as nicotine, alcohol or hot spices. If you also have an allergy or food intolerance, it is helpful to follow an elimination diet. This helps to quickly identify foods that are stressful.
Afterwards, you should completely eliminate them from your diet. We advise men and women with psoriasis to try a gluten-free diet. It does not matter if you actually have gluten intolerance (coeliac disease).
Psoriasis and the microbiome.

Bacteria and fungi colonise the skin and all mucous membranes of our body. These useful helpers train the human immune system in the intestine and supply the organism with vital micronutrients. No wonder that intestinal dysbiosis is associated with numerous diseases.
Stool tests of patients with psoriasis indicate a massive dysbiosis of the intestine. Some scientists see this as the reason for the frequent co-occurrence of psoriasis and chronic inflammatory bowel diseases (Crohn’s disease, ulcerative colitis). In this context, the increased permeability of the intestine (leaky gut) seems to play an important role.28,29
As a group of French researchers found in 2018 using animal studies, taking beneficial gut bacteria (probiotics) can reduce the amount of inflammation in the skin.30
What role does the psyche play in psoriasis?
I’m going off the deep end, I’m not itching, it’s getting under your skin: phrases like these suggest a connection between our psyche and the outer shell of our body. In the following, we will go into detail about the connections.
Our skin as a mirror of the soul.
Why psoriasis is more than a skin problem is explained by Prof. Dr. Uwe Gieler, senior clinical physician at the Department of Psychosomatics and Psychotherapy at the University Hospital Giessen and Marburg (UKGM): “The skin and the central nervous system have the same developmental origin. Both are formed in humans from completely identical predispositions.”31
Psychotherapists refer to skin diseases such as psoriasis, neurodermatitis, herpes and acne as psychosomatic dermatoses. In other words, these diseases arise on a physical level but are influenced by the psyche.
The Austrian psychologist and psychotherapist Dr Elisabeth Adleff provides the following explanation: “Psoriasis and the accompanying skin symptoms usually have something to do with how we are organised with regard to our own boundaries: If we ensure – consciously or unconsciously – a good regulation of closeness and distance on a psychological level, we are in balance in this respect.
If there is an imbalance, the psyche begins to express itself more and more through the body. The body develops different symptoms to indicate the imbalance.”32
Stress can increase the symptoms of psoriasis.
Our body reacts to stressful situations. The reason is rooted in evolution: In dangerous situations, our ancestors had to make a lightning-quick decision between fight and flight. Stress signals activate the so-calledhypothalamic-pituitary-adrenal axis (HHN axis) and the sympathetic nervous system.
These in turn cause the release of stress hormones and neuropeptides, which above all influence our immune system. Several studies have shown that the skin is particularly sensitive to psychological stress.33
It is no wonder that people with psoriasis under psychological stress have been shown to have an increased number of inflammatory markers in their blood. More than half of the sufferers confirm that stressful situations, everyday annoyances or drastic life events aggravate their symptoms. If sufferers ignore the stress, relapses are more frequent and more severe.34
Psoriasis patients quickly get into a vicious circle.
Because of the noticeable skin manifestations, psoriasis patients are often apprehensive about exposing themselves to others. In their eyes, the changes appear much more dramatic than an uninvolved observer would perceive them. Many people with psoriasis believe they are disfigured and unconsciously devalue themselves.
Because of the noticeable skin manifestations, psoriasis patients are often apprehensive about exposing themselves to others. In their eyes, the changes appear much more dramatic than an uninvolved observer would perceive them. Many people with psoriasis believe they are disfigured and unconsciously devalue themselves.
Another issue is the rejection and stigmatisation that some sufferers experience. As a result, quality of life, general health and functioning in society are impaired. Subtle coping mechanisms are at work that can lead to depression, anxiety and loss of confidence. In many cases, the psychological problems associated with psoriasis significantly exceed the physical burden.36,37
Psoriasis – what can I do?

Stress reduction as well as the “right attitude” towards your skin are the be-all and end-all of treatment from a psychological point of view. Try to find out the reasons why your mind builds up a shell – similar to that of a turtle – against the environment. You obviously have trouble separating yourself from other people. And this is exactly what you should work on with the help of an experienced psychotherapist.
The ÁYIO-Q Centre of Vitality offers various solutions. Among other things, the ÁYIO-Q Pnoē-Therapy. Eliminate stress within minutes. If you would like to know more about your life energy and the state of your self-healing powers, it is best to take the free self-test on our website.
FAQ
Does psoriasis weaken the immune system?
In psoriasis, the immune system attacks an endogenous protein in the skin. Conventional medical therapy therefore uses immunosuppressants, among other things, which deliberately suppress the body’s defences. Thus, it is not the psoriasis that weakens the immune system, but the treatment by the doctor.
Is psoriasis the same as neurodermatitis?
Although both are inflammatory skin diseases, psoriasis and neurodermatitis have nothing to do with each other. Neurodermatitis, like hay fever, house dust allergy and asthma, belongs to the so-called atopic group.
The symptoms are triggered by an excessive reaction of the immune system to harmless substances (allergens) that enter the body from outside. Psoriasis, on the other hand, is an autoimmune disease in which the body’s defences are directed against its own cells or tissue.
Why does psoriasis itch?
The itching occurs because of the inflammation in the affected areas of the skin. When you scratch, the nerve endings in the skin become larger and therefore more sensitive. As a result, the itching continues to increase.
Is there psoriasis that doesn’t itch?
Two thirds of psoriasis patients suffer from a mild form of the disease. For some sufferers, the itching is only mild or even absent.
Why is psoriasis not curable?
Since the disease has a genetic cause, the predisposition remains lifelong. With the help of appropriate treatments, possible triggers and other cofactors such as the microbiome in the gut can be influenced. This may also reduce the frequency of psoriasis episodes.
Sources:
[1] Psoriasis, at https://www.netdoktor.de, accessed 10.11.21
[2] Nail psoriasis, at https://www.psoriasis.info, accessed 10.11.21
[3] Bathing regulations discriminate again – or still?!, at https://www.psoriasis-bund.de, accessed 10.11.21
[4] Psoriasis: Causes, Symptoms, Treatment, at https://www.deutsche-familienversicherung.de, accessed 10.11.21
[5] What is psoriasis?, at https://www.psoriasis-bund.de, accessed 10.11.21
[6] Carrascosa JM et al. Obesity and psoriasis: inflammatory nature of obesity, relationship between psoriasis and obesity, and therapeutic implications. Actas Dermosifiliogr. Jan-Feb 2014;105(1):31-44.
[7] Psoriasis dandruff and itching under control, at https://www.aerztezeitung.de, accessed 10.11.21
[8] Naldi L et al. Diet and physical exercise in psoriasis: a randomized controlled trial. Br J Dermatol. 2014 Mar;170(3):634-42.
[9] Castaldo G et al. Aggressive weight-loss program with a ketogenic induction phase for the treatment of chronic plaque psoriasis: A proof-of-concept, single-arm, open-label clinical trial. Nutrition. 2020 Jun;74:110757.
[10] Lin X, Huang T. Oxidative stress in psoriasis and potential therapeutic use of antioxidants. Free Radic Res. 2016 Jun;50(6):585-95.
[11] Péter I et al. Psoriasis and oxidative stress. Orv Hetil. 2016 Nov;157(45):1781-1785.
[12] Ramadan R et al. The antioxidant role of paraoxonase 1 and vitamin E in three autoimmune diseases. Skin Pharmacol Physiol. 2013;26(1):2-7.
[13] Oxidativer Stress, auf https://www.meine-gesundheit.de, Zugriffszeitpunkt 29.10.21
[14] Pujari VM et al. The serum levels of malondialdehyde, vitamin e and erythrocyte catalase activity in psoriasis patients. J Clin Diagn Res. 2014 Nov;8(11):CC14-6.
[15] Kirmit A et al. Trace elements and oxidative stress status in patients with psoriasis. Postepy Dermatol Alergol. 2020 Jun;37(3):333-339.
[16] Kharaeva Z et al. Clinical and biochemical effects of coenzyme Q(10), vitamin E, and selenium supplementation to psoriasis patients. Nutrition. 2009 Mar;25(3):295-302.
[17] Barrea L et al. Vitamin D and its role in psoriasis: An overview of the dermatologist and nutritionist. Rev Endocr Metab Disord. 2017;18(2):195-205.
[18] Stanescu AMA et al. Oral Vitamin D Therapy in Patients with Psoriasis. Nutrients. 2021 Jan 6;13(1):163.
[19] Wu AG, Weinberg JM. The impact of diet on psoriasis. Cutis. 2019 Aug;104(2S):7-10.
[20] Barrea L et al. Nutrition and psoriasis: is there any association between the severity of the disease and adherence to the Mediterranean diet? J Transl Med. 2015 Jan 27;13:18.
[21] Phan C et al. Association Between Mediterranean Anti-inflammatory Dietary Profile and Severity of Psoriasis: Results From the NutriNet-Santé Cohort. JAMA Dermatol. 2018 Sep 1;154(9):1017-1024.
[22] Ingkapairoj K et al. Dietary habits and perceptions of psoriatic patients: Mediterranean versus Asian diets. J Dermatolog Treat. 2021 Aug 9;1-7.
[23] Caso F et al. Mediterranean diet and Psoriatic Arthritis activity: a multicenter cross-sectional study. Rheumatol Int. 2020 Jun;40(6):951-958.
[24] Kanda N et al. Nutrition and Psoriasis. Int J Mol Sci. 2020 Jul 29;21(15):5405.
[25] Balić A et al. Omega-3 Versus Omega-6 Polyunsaturated Fatty Acids in the Prevention and Treatment of Inflammatory Skin Diseases. Int J Mol Sci. 2020 Jan 23;21(3):741.
[26] Clark CCT et al. Efficacy of ω-3 supplementation in patients with psoriasis: a meta-analysis of randomized controlled trials. Clin Rheumatol. 2019 Apr;38(4):977-988.
[27] Korinek M et al. Anti-Inflammatory and Antimicrobial Volatile Oils: Fennel and Cumin Inhibit Neutrophilic Inflammation via Regulating Calcium and MAPKs. Front Pharmacol. 2021 Oct 11;12:674095.
[28] Menzel I, Holzmann H. Reflections on seborrheic scalp eczema and psoriasis capillitii in relation to intestinal mycoses. Z Hautkr. 1986 Apr 1;61(7):451-4.
[29] Myers B et al. The gut microbiome in psoriasis and psoriatic arthritis. Best Pract Res Clin Rheumatol. 2019 Dec;33(6):101494.
[30] Holowacz S et al. Lactobacillus salivarius LA307 and Lactobacillus rhamnosus LA305 attenuate skin inflammation in mice. Benef Microbes. 2018 Feb 27;9(2):299-309.
[31] Sonnenmoser M. Hautkrankheiten: Wechselwirkung zwischen Haut und Psyche. Deutsches Ärzteblatt PP. Ausgabe November 2002, Seite 501.
[32] Psoriasis – Spiegel der Seele, auf https://www.hautinfo.at, Zugriffszeitpunkt 10.11.21
[33] Hall JMF et al. Psychological Stress and the Cutaneous Immune Response: Roles of the HPA Axis and the Sympathetic Nervous System in Atopic Dermatitis and Psoriasis. Dermatol Res Pract. 2012;2012:403908.
[34] Scalp – Stress, at https://www.psoriasis.info, accessed 10.11.21
[35] The skin as a mirror of the sore soul, at https://www.psoriasis-netz.de, accessed 10.11.21
[36] Petit V et al. Stigmatization in psoriasis patients. Pol Merkur Lekarski. 2014 Nov;37(221):301-4.
[37] Khawaja AR et al. Disease Severity, Quality of Life, and Psychiatric Morbidity in Patients With Psoriasis With Reference to Sociodemographic, Lifestyle, and Clinical Variables: A Prospective, Cross-Sectional Study From Lahore, Pakistan. Prim Care Companion CNS Disord. 2015 Jun 25;17(3):10.4088/PCC.14m01629.