Updated on 21. April 2022 from ÁYIO-Q Redaktion
Reading time: approx. 15 minutes
Voices that no one else hears – An attack on the self
Schizophrenia is a mental illness characterised by a loss of perception of facts (psychosis), hallucinations (usually hearing voices), delusions, thought states and also unusual behaviour, a reduced expression of sensations, listlessness, a decrease in mental capacity (cognition) and disabilities in social and professional life and also in self-care. According to this, about 24 million people worldwide, i.e. 1 in 300 people, are affected by this psychosis.
Do you hear voices that are not real, move reflexively and have violent reactions to other people? People suffering from schizophrenia usually fulfil many requirements of our classic prejudice of a crazy person. To this day, they also suffer from stigmatisation by our society. In this article, learn what exactly schizophrenia is, how to recognise it and how to deal with it.
- Description
- Symptoms
- Causes & Risk Factors
- Incidence & Effects
- Diagnosis
- Forecast
- Conventional Medicine Treatment
- Natural & Complementary Therapies
What does it mean to struggle with schizophrenia?
Schizophrenia is a common health problem worldwide. It usually affects young people who are in the process of becoming independent and can lead to lifelong impairment as well as prejudice. In terms of cost, schizophrenia is one of the most significant forms of illness.
Schizophrenia is seen in about 1 per cent of the population, both men and women. In the US, schizophrenia accounts for 1 in 5 days of leave and about 2.5% of total health insurance costs. Schizophrenia is much more common than Alzheimer’s disease and multiple sclerosis.
It is usually difficult to determine the exact time of onset of schizophrenia, as not knowing the symptoms can delay clinical treatment for years. The disorder may begin in the teenage years or later in life.
When the ability to cope with everyday social life declines, this can lead to drug use, distress and homelessness. Sufferers with untreated schizophrenia break off contact with family members and friends and often live on the streets of large cities. The illness can last a lifetime, and in most cases psychosocial functioning is also impaired for life.
What are the signs and symptoms of schizophrenia?
Schizophrenia can start unexpectedly, within days and weeks, or slowly and insidiously over years. The extent and nature of symptoms vary among individuals, but are usually severe enough to impair the ability to function, socialise with others and care for oneself.
However, sometimes the symptoms are mild at the beginning (called the prodromal stage). Patients may simply seem withdrawn, disorganised or suspicious. Medical professionals may already identify the symptoms as the beginning of schizophrenia. Sometimes, however, the picture only comes together gradually.
Schizophrenia is recognisable by psychotic symptoms such as delusions, hallucinations, confused thinking and speech, and unusual and inappropriate behaviour. Psychotic signs also include loss of facts.
Some people with schizophrenia experience a deterioration in psychological (cognitive) abilities that regularly occurs at the beginning of the illness. These cognitive problems lead to difficulties in concentration, abstract thinking and problem solving. The intensity of the cognitive problems largely determines the degree of disability of persons with schizophrenia. Many persons with schizophrenia are unemployed and have little or no contact with family members or others.
Signs and symptoms can be triggered or made worse by stressful events, such as losing a job or ending a close relationship. Drug use (including marijuana) can also trigger or worsen the signs and symptoms.
Essential: A number of conditions, such as thyroid problems, abnormal brain growth, seizure disorders (such as esilepsy) and other mental illnesses, can cause signs and symptoms similar to those of schizophrenia.
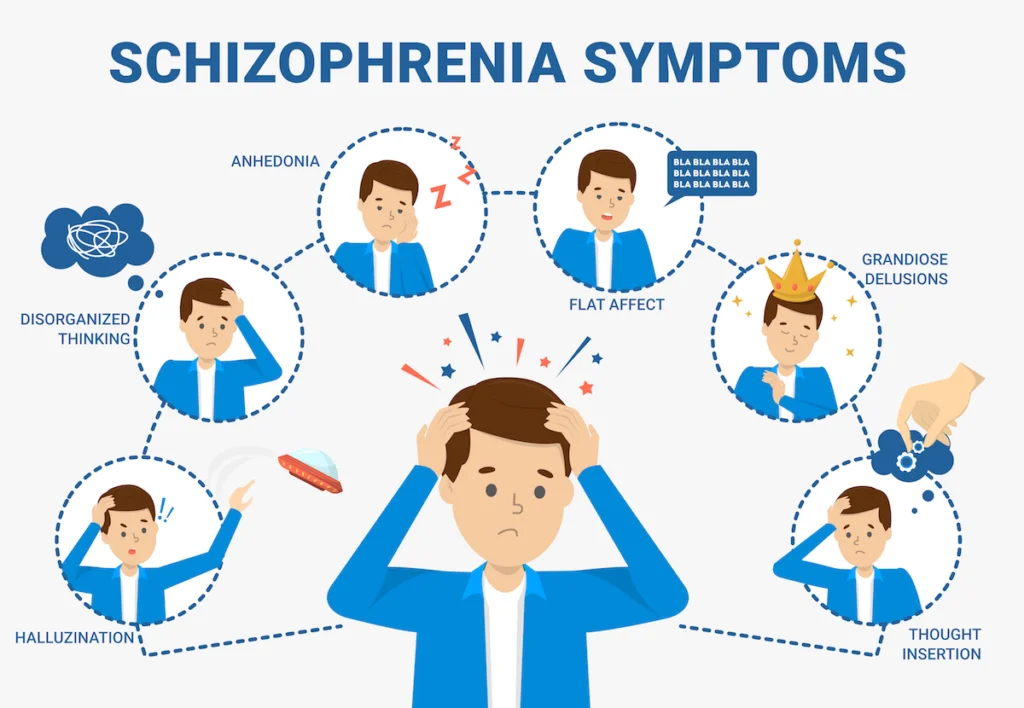
In general, the signs and symptoms of schizophrenia can be divided into four main groups:
- Positive symptoms
- Negative symptoms
- Disorganisation
- Cognitive deficits
Affected people may show signs and symptoms from one or all of the groups.
Positive symptoms
Positive symptoms include a disturbance (distortion) of normal functions. These include the following:
- Delusions are misconceptions and are usually accompanied by a misinterpretation of knowledge or experience. Patients hold on to these beliefs even though there is clear evidence to the contrary. There are multiple manifestations of delusions. For example, people with schizophrenia may suffer from delusions of persecution and think that they are being tortured, abused, tricked or spied on. Patients with partnership delusions believe that sections of books, newspapers or even melodies are specifically targeted at them. In belief withdrawal or thought inspiration, patients think that their ideas can be read, that their thoughts are transferred to others, what thoughts and also impulses are fed to them from outside. Delusions in schizophrenia can be grotesque, but do not have to be. Striking delusions are clearly doubtful and also cannot be derived from experiences in daily life. Patients believe that someone has removed their internal organs without leaving a scar. Non-bizarre delusions include scenarios that may actually occur in everyday life, such as being stalked or cheated on by one’s (life partner’s) companion.
- Hallucinations include hearing, seeing, tasting or literally feeling things that others cannot hear or see, and so on. The most typical hallucinations have to do with hearing (auditory hallucinations). Sufferers often hear voices commenting on their habits, talking to each other or making substantial and offensive statements.
Negative symptoms
Negative symptoms consist of a restriction or loss of normal functions. These include the following:
- Few or no feelings show in diminished mental expression (“flat affect”). They do not use their hands or head to communicate their feelings when speaking.
- The absence of speech refers to a reduced need to speak. Questions can be answered extremely quickly with one or two words, giving the impression of an inner emptiness.
- Anhedonia describes a reduced ability to feel pleasure. Sufferers usually show little interest in previous tasks and spend their time on purposeless activities.
- Anti-sociality refers to a lack of interest in social partnerships.
These unfavourable signs are usually associated with a general loss of motivation and goals, as well as a feeling of aimlessness.
Disorganisation
Disorganisation includes thought disorders and bizarre behaviour:
- A thought disorder refers to a disorganised way of thinking that manifests itself in someone digressing and switching from one topic to another. Expression may be slightly disorganised or completely incoherent and incomprehensible.
- Bizarre behaviour can take the form of childish silliness and excitement or be characterised by inappropriate appearance, hygiene or behaviour. The catatonia is an extreme form of bizarre behaviour. In this case, the sufferer adopts a rigid posture and resists attempts to encourage him to move or, on the contrary, moves aimlessly.
Cognitive deficits

Cognitive deficits describe the difficulties people have in concentrating, remembering, organising and planning, and solving problems. Some are unable to focus on reading a book, understand the plot of a film or television programme, or follow instructions. For others, it is impossible to ignore distractions or concentrate on a task for a long period of time. Therefore, a job that requires attention to detail, is characterised by complex processes and involves decision-making may be unsuitable.
Suicide
About 5 to 6 percent of people with schizophrenia commit suicide, about 20 percent attempt suicide, and many more have significant self-destructive ideation. Suicide is the main reason for premature death in people with schizophrenia and one of the reasons why schizophrenia reduces average life expectancy by ten years.
Boys with schizophrenia are at increased risk of suicide, especially if they are also suffering from drug dependence. In addition, the danger increases in people with depressive signs and symptoms or feelings of despair, who are unemployed or who have just undergone psychosis or who have been discharged from hospital.
The greatest risk of suicide is in people who developed schizophrenia later in life and who were well before. These people still have the capacity to feel sorrow and suffering. This makes them particularly prone to acts of fear because they know the effects of their illness. For these people, the chances of recovery are better than for others.
violence
Contrary to popular belief, schizophrenic people are only at low risk of becoming violent. Threats of violence and small hostile outbursts are much more common than seriously dangerous behaviour. Very few significantly clinically depressed, isolated, paranoid people hit or eliminate others whom they hold solely responsible for their problems (e.g. an authority figure, an acquaintance, a partner).
The following people are most likely to be very violent:
- People who use alcohol or recreational drugs
- Those with delusions of being persecuted
- Persons with hallucinations in which they are made to commit wild acts
- People who do not take their recommended medication
However, even taking risk aspects into account, it is difficult for medical professionals to accurately predict whether a particular person with schizophrenia will be involved in violent acts.
What are the possible causes and risk factors for schizophrenia?
According to the current state of scientific research, experts assume that numerous elements are possible causes of schizophrenia.
- Hereditary factors: Susceptibility to schizophrenia, but not the disease itself, appears to be hereditary.
- Susceptibility: Many sufferers are unable to fully protect themselves from environmental influences. This can be both caused and exacerbated by various elements such as hereditary predisposition, brain injury, stressful childhood experiences, tension or drug use.
- Triggering factors: However, the onset of the illness only occurs when life events occur that the affected person can no longer cope with. Drug use can also be a trigger for schizophrenia. As a rule, several elements must interact.
- Changes in brain structure: Studies show that the brain structure of schizophrenics differs from that of healthy and balanced people. How these abnormalities, e.g. in the limbic system, which is also responsible for our mental actions, affect the disease still needs to be further investigated.
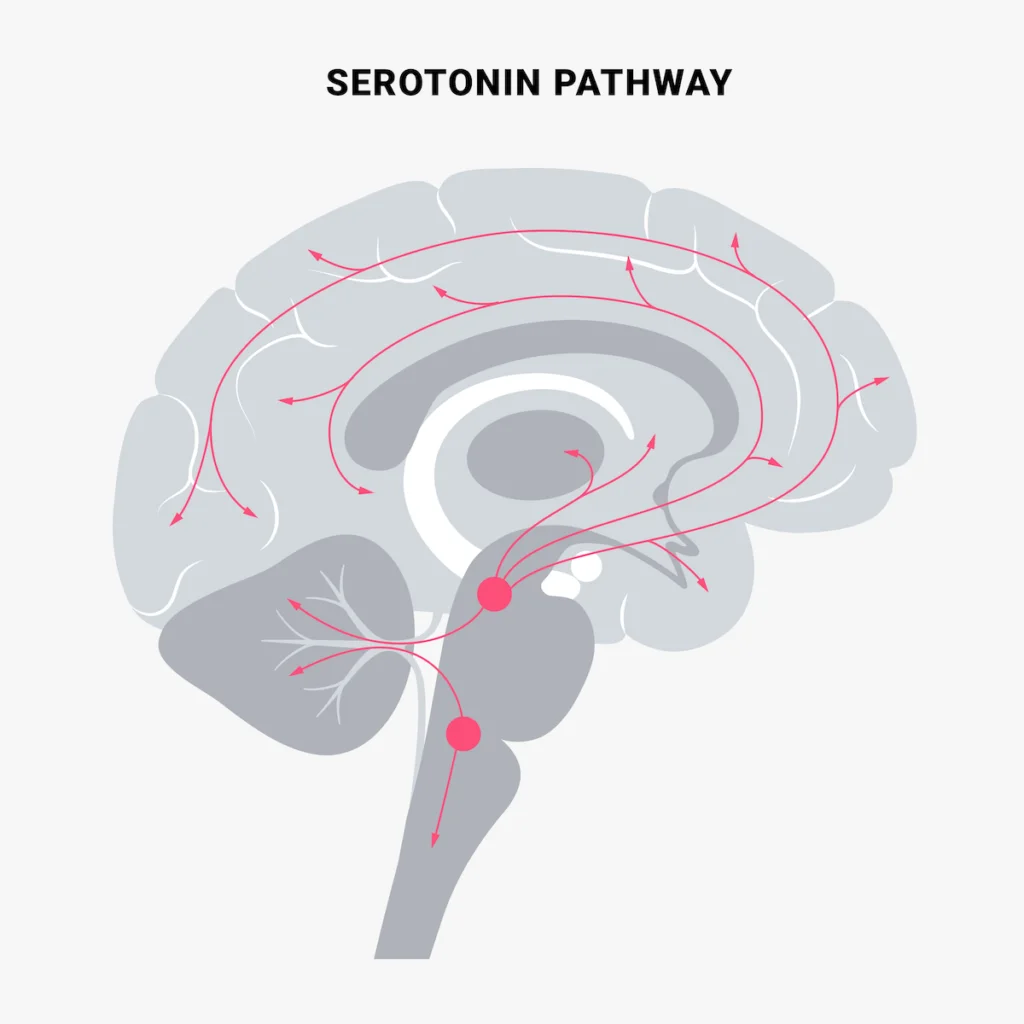
- Natural messengers: The hormone neurotransmitter dopamine appears to play a major function in the brain. The neurotransmitter sends signals from one nerve cell to the next. In schizophrenic people, an excess of the natural messenger dopamine can be detected. Various other messenger systems (e.g. the serotonin system) are apparently also involved in the disorder.
- Stress and stressful experiences are likely to be particularly stressful for people with schizophrenia. Even before the onset of the illness, they often find it difficult to cope with difficult circumstances. At a certain point, the stress becomes too much. Then the stress becomes the trigger that sets off the health problem. Many schizophrenic people report important life events before the onset of the illness. This can be, for example, the loss of a close person or a problematic professional situation. But positive situations can also trigger stress – for example, a wedding celebration or the birth of a child.
For people with a schizophrenic mother or father or a schizophrenic sibling, the risk of developing schizophrenia themselves increases to 10%, compared to 1% for the normal population. In a pair of twins, the probability that one of the twins will develop schizophrenia is 50% for the other twin. This speaks for a hereditary component.
Incidence and impact of schizophrenia
Weltweit sind etwa 24 Millionen Menschen von Schizophrenie betroffen, also 1 von 300 Personen (0,32 %). Bei den Erwachsenen liegt dieser Anteil bei 1 von 222 Personen (0,45 %). Sie tritt nicht so häufig auf wie verschiedene andere psychische Erkrankungen. Der Beginn ist am häufigsten in den späten Teenagerjahren und in den Zwanzigern, und der Beginn ist bei Männern tendenziell früher als bei Frauen.
Bei Personen mit Schizophrenie ist die Wahrscheinlichkeit, dass sie früher sterben als die Allgemeinbevölkerung, 2 bis 3 Mal höher. Dies ist in der Regel auf körperliche Erkrankungen wie Herz- und Stoffwechselkrankheiten sowie auf übertragbare Krankheiten zurückzuführen.
Menschen mit Schizophrenie erleben in der Regel Menschenrechtsverletzungen sowohl in psychiatrischen Einrichtungen als auch in der Umgebung. Stigmatisierung von Menschen mit dieser Störung ist äußerst ausgeprägt und weit verbreitet, was zu sozialer Ausgrenzung führt und ihre Beziehungen zu anderen Menschen, insbesondere zu Familie und Freunden, beeinträchtigt. Dies verschärft die Diskriminierung, was wiederum den Zugang zur allgemeinen Gesundheitsversorgung, zur Bildung, zu Wohnraum und auch zur Arbeitswelt einschränken kann.
Humanitarian and health emergencies can lead to extreme anxiety and fear, failure of social support, isolation and disruption of health care and medication. These changes can affect the lives of people with schizophrenia, for example by worsening existing signs and symptoms. In emergencies, people with schizophrenia are much more at risk than others of various civil rights violations, such as being forgotten, abandoned, homeless, abused and excluded.
Medical diagnosis of schizophrenia
A prerequisite for the diagnosis of schizophrenia is that the standards explained below have actually existed for at least 4 weeks or longer. The doctor asks about these in a detailed conversation. Some symptoms are not noticed by the affected person themselves. Family members or other caregivers can often provide information.
Additional examinations are very important to rule out diseases with similar signs and symptoms, e.g. a specific metabolic disorder or alcohol and drug abuse.
In order to be able to make a medical diagnosis of schizophrenia, a comprehensive discussion with the affected person is essential. The mental signs and symptoms that occur are discussed in detail. There are certain requirements for this as well as special clinical examinations. The leading symptoms that are asked about are defined in the ICD-10 for schizophrenia:
- Thought excitation, thought invocation, thought withdrawal, thought propagation
- Misperceptions of control or influence; feeling made in relation to bodily movements, thoughts, tasks or sensations; delusional ideas.
- Voices commenting on or leading dialogue
- consistent, culturally inappropriate or completely impractical misunderstandings (strange misunderstandings)
- constant hallucinations of any kind of sensory modality
- Believed tearing off or inserting directly into the thought cycle
- comatose symptoms such as anxiety, postural stereotypies, negativism or wonderment
- Negative signs and symptoms such as conspicuous lethargy, impoverishment of speech, “flat affect”.
For a diagnosis of “schizophrenia”, at least one clear sign (or 2 or even more signs and symptoms if they are less clear) of groups 1 – 4 or at least two signs and symptoms of groups 5 – 8 must occur, almost continuously for a month or even longer.
What is the prognosis for schizophrenia?
Early detection and early therapy are the guidelines for the treatment of schizophrenia. The earlier treatment is started, the better the final outcome.
Since schizophrenia patients have been treated with a combination of neuroleptics and psychotherapy, the prognosis of the disease has improved considerably. About 20 to 25 percent of patients are completely cured by this treatment. But even if patients are not completely cured, outpatient treatment is often sufficient for them to lead a largely normal life despite their schizophrenia. The social environment has a great influence on this: if those affected experience a lot of understanding and also support from relatives, this can have a favourable influence on the course of the illness.
Note: Unlike tranquillisers, neuroleptics are not addictive – either physically or psychologically.
Over time, the prognosis varies:
- One third of those affected improve significantly and permanently
- Another third achieve some improvement with occasional episodes and recurrent disability
- One third experience extreme and long-term impairments
Only about 15 percent of all people with schizophrenia cope better than before the onset of schizophrenia.
Factors that have a much better prognosis:
- Sudden onset of signs and symptoms
- Older age at onset of symptoms
- Good skills and also abilities before the onset of the disease
- Only mild cognitive impairment
- Visibility of only a few unfavourable signs and symptoms (such as reduced psychological expression).
- A much shorter time span between the first psychotic episode and therapy
Factors showing a much worse prognosis:
- Younger age at onset of symptoms
- Impairment in social situations as well as at work before the onset of the disease
- Domestic predisposition to schizophrenia
- Visibility of multiple negative symptoms
- A long period between the very first psychotic episode and treatment
The prognosis is less favourable in men than in women. Women respond much better to therapy.
Drug therapy for schizophrenia
Different groups of medications can be used to treat schizophrenia, depending on the form and severity of the symptoms:
- Neuroleptics (antipsychotics): They were the first effective drugs for the treatment of psychosis. By interfering with the metabolic process of nerve messengers, they reduce states of tension and anxiety, delusions and also hallucinations. In the process, however, neuroleptics have extreme negative effects such as muscle stiffness, tremors, muscle twitching, numbness, fatigue, apathy and also reduced reaction time.
- Atypical neuroleptics: These further developments of the “timeless” neuroleptics work much better and have fewer negative effects. Recognised active substances are risperidone and clozapine.
- Antidepressants: In addition to antipsychotics (classical or atypical neuroleptics), the doctor occasionally recommends antidepressants. This makes sense for schizophrenia patients who are also listless. Antidepressants have a favourable effect on mood, drive and performance.
- Sedatives: During an acute psychotic stage, some people struggle with severe anxiety. In this case, tranquillisers can help. However, as they are addictive, they are used only for a short time if possible.
Psychotherapy for schizophrenia
Psychiatric therapy is becoming increasingly important for the treatment of schizophrenia. It can have a positive influence on the course of the disease in the long term. Typically, cognitive behaviour modification is used. Important aspects of psychotherapeutic therapy are:
- Reducing stress and anxiety through details: First of all, it is important to relieve the affected person’s fear of the illness by providing them with detailed information about schizophrenia. Family members also benefit from more knowledge, for example, by being more understanding and supportive of the person with schizophrenia. Communication training is also helpful, as it makes it easier to deal with the client.
- Dealing with stress and difficult scenarios: In the treatment, the client learns, among other things, how to better deal with difficult situations that can aggravate their symptoms. A central aspect of this is dealing with stress.
- Dealing with frightening experiences: With the help of emotional schizophrenia treatment, the client can also deal much better with the frightening experiences he had during the acute phases of the illness. This supports him in general.
- The person also learns to recognise the early warning signs of a schizophrenic episode. These can be very different. Often, for example, disturbances of the peace or extreme irritability herald a new episode. Then it is important to lower the sources of tension in consultation with the doctor and possibly increase the medication dose for a short time.
Help after hospitalisation
After an inpatient stay, the person concerned usually needs support at home as well. Social pedagogues take on this task. They help the person concerned to find their way in everyday life again.
For many patients, it is a particular challenge that their ability to concentrate, their functioning memory and their ability to plan ahead are impaired by the disease. In this case, cognitive therapy can help. It works together with behavioural therapy methods and also with special computer system training. This increases the likelihood that the patient will be able to work again. In addition, insight into the disease and adherence to therapy are strengthened.
5 Complementary treatments for schizophrenia
The terms “complementary” and “alternative” are usually used synonymously. Nevertheless, these terms describe two different types of therapies. The term “complementary” refers to treatments that are not traditional and are also used in combination with traditional treatments. The term “alternative” treatment is used when clinical treatments that are not mainstream are used instead of traditional medicines.
Medication is necessary in the therapy of schizophrenia. Appropriate therapies with medication should not replace the care of a doctor. Talk to your doctor before using an alternative therapy method to find out if it is risk-free.
1. Vitamins In Schizophrenia
According to the non-profit organisation Food for the Brain people with schizophrenia usually have reduced levels of folic acid or vitamin B9 in their blood. Taking folic acid supplements can relieve the symptoms. In a 2014 report on a research study researchers note that B vitamins, including vitamins B12 and B6, may also be beneficial. Several studies used a mixture of these vitamins.
The research report also examined some small studies that recommend that vitamins C and E may be beneficial. The report concludes that more studies should be done. Some research has linked vitamin D deficiency, especially at a young age, to schizophrenia.
In 2012, Indian researchers conducted an evaluation of the studies published until then on the topic of “vitamins and schizophrenia”. They also found that people with mental illnesses who also have a vitamin deficiency subsequently have to struggle with more severe symptoms than patients with a good supply of essential substances. Furthermore, patients with vitamin deficiencies respond less well to conventional treatment. Vitamins B, C, D and E in particular play a crucial role in the development of schizophrenia.
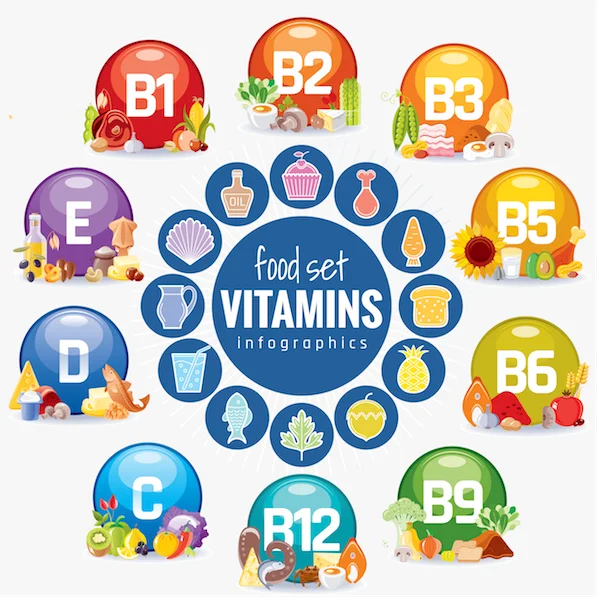
Thus, vitamin deficiencies play a significant role in schizophrenia. They increase the risk of developing schizophrenia in the first place and cause the symptoms to get worse and worse when the disease is already there. At the same time, of course, vitamin deficiencies not only worsen the symptoms of schizophrenia, but also lead to all the other problems associated with the particular vitamin deficiency, be it cardiovascular problems, persistent inflammatory diseases, disorders of lipid metabolism, etc.

In every case of schizophrenia – whether you are affected yourself or have relatives – the following vitamins should be investigated and administered in sufficient doses (together with the above-mentioned medication groups, if necessary):
B vitamins for schizophrenia – support the effect of conventional medical therapy;
Hoffer’s adrenochrome thesis as well as high doses of vitamin B3 are currently rejected and additionally excluded in the existing received clinical treatment for schizophrenia. However, a meta-analysis published in February 2017 confirms Hoffer’s technique and also shows that high doses of B vitamins along with basic therapy appear to produce dramatically better results in reducing schizophrenia symptoms than standard therapy alone.
The study, conducted by Joseph Firth’s group from the College of Manchester in the UK, was published in the journal Psychological Medication. In it, Firth and his colleagues evaluated all the studies that had investigated the effect of vitamins and minerals on schizophrenia. This involved a total of 18 research studies involving 832 people, every single one of whom was currently receiving psychiatric therapy.
Vitamin C in schizophrenia
In one study, schizophrenic individuals on the same diet had significantly lower plasma vitamin C levels as well as lower urinary vitamin C excretion than the non-schizophrenic control group. Only after the schizophrenic participants were given a daily dose of 70 mg vitamin C for four weeks, no differences were found between the two groups, at least as far as plasma levels were concerned. However, the vitamin C levels in the urine were still decreased.
Subsequently, the schizophrenic subjects were offered 1 g of vitamin C daily – for four weeks. Only now did all vitamin C values correspond to those of the control group. The scientists involved mentioned that their study confirmed the theory that people with schizophrenia have a much higher vitamin C requirement than healthy people.
In a double-blind, placebo-controlled research study, the scientists were able to prove that taking vitamin C supplements for eight weeks lowered oxidative stress and also improved psychological symptoms. A total of 20 people took part in each of the two groups. All subjects were initially found to have both high MDA levels (a sign of oxidative stress and anxiety) and reduced vitamin C levels. After taking vitamin C (together with the recommended antipsychotic), both values increased – but only in the vitamin C group, not in the group with the sugar pills. At the same time, the symptoms of schizophrenia decreased significantly.
Vitamin E in schizophrenia
Vitamin E is a widely known antioxidant that prevents damage from cell-damaging free radicals. Vitamin E is used in psychiatry, for example, for tardive dyskinesia which occurs in 20 per cent of all people who have been treated with antipsychotics for many years. The vitamin E can stop the tardive dyskinesia or reduce its intensity – the latter especially if the dyskinesia has only occurred in the last 5 years.
After reviewing the available documentation, one can conclude that an excellent supply of vitamin E, vitamin C and beta-carotene – preferably in the early stages of the disease – can prevent further oxidative damage and thus enhance the scenario.
In a double-blind placebo-controlled research study, high doses of pyridoxine (vitamin B6) (400 mg/day) were used. This minimised the signs and symptoms of tardive dyskinesia in schizophrenia patients. As soon as the vitamin was discontinued after a few weeks, the symptoms returned with increased intensity.
2. Fatty Acids In Schizophrenia
Dietary supplementation with fish oil
Fish oil is a rich source of omega-3 fatty acids. These nutrients are known to reduce inflammation in the body. Inflammation can play a role in many mental disorders, including schizophrenia. In a study involving 81 young people at high risk of schizophrenia, those who took fish oil supplements were less likely to develop schizophrenia. The results are encouraging, but much more research is needed.
It is not clear whether fish oil supplements increase signs and symptoms in people who have already been diagnosed with schizophrenia. However, there may be other benefits. One of these is improved heart health. For example, the National Partnership on Mental Disease notes that people with schizophrenia are at higher risk for metabolic disorders. This in turn increases the risk of heart disease. Some people choose to take omega-3 fatty acids simply for the heart health benefits.
3. Management Of The Nutrition Plan
In some studies a gluten-free diet has been found to reduce the signs and symptoms of schizophrenia, but the benefits have only been seen in a specific subgroup of people. Gluten is a component of certain grains, particularly wheat. Studies on ketogenic diet plans have also shown encouraging results. A ketogenic diet plan is a high-fat, low-carbohydrate diet that also includes protein-rich foods. However, dietary changes do not always make a difference in people with schizophrenia. More research studies are needed to determine if there is a link between diet and schizophrenia.
Always talk to your doctor before making any significant changes to your diet. A change in diet must not be used as a substitute for medication.
Traditional Chinese Medicine (TCM)4;
Wen Dan Tang
The Chinese bioformula Wen Dan Tang (WDT) may be helpful for people with schizophrenia. This is according to a meta-study from the Cochrane Database conducted by Chinese authors who analysed 15 randomised trials involving 1437 participants. The results showed that WDT could have some helpful results on the short-term global outcomes and psychological state of people with schizophrenia compared with placebo or no treatment. WDT was found to be non-inferior to antipsychotic medications (such as chlorpromazine or risperidone) in terms of global outcomes and psychological state, and was also associated with fewer side effects. When WDT was combined with a reduced dose of antipsychotic medication, positive results were found in terms of global and psychological state, and adverse effects were also reduced.
5. Meditation In Schizophrenia
Meditation transforms the brain
Regular meditation leaves a permanent mark on our mind: it completely prevents activity in the centres of the brain that are the cause of anxiety, mental illness and also attention deficit disorder.
The brain areas of people who meditate consistently are more connected. As a result, they are better able to focus on a present situation or tasks in daily life and are much more mindful. This is reported by US researchers in the journal Proceedings of the National Academy of Sciences.
“The ability of meditation to help people live in the here and now has actually been known for hundreds of years,” explains lead author Judson A. Maker from Yale College. The same goes for the fact that normal meditation has a positive effect on general well-being: “It helps with pain, depression, stress and anxiety, helps smokers and other addicts quit, and can also protect against diseases like shingles,” says the researcher. However, the psychological changes behind these effects are only partially known so far, he adds.
Excessive obsession with one’s own inner world makes one ill
But too much activity in the regions dampened by meditation is additionally considered a danger aspect for schizophrenia, attention deficit disorders like ADHD and anxiety. “Characteristic of many types of mental illness is a pathological preoccupation with one’s own thoughts and feelings,” says Maker.
He claims the research study has now actually shown that meditation affects mechanisms underlying these problems in the brain. “This raises the tantalising possibility that we can alleviate ADHD and other conditions through a technique as simple and inexpensive as meditation,” the researchers write.
Finally: Details for family members
When a person falls ill with schizophrenia, it is very difficult for the relatives. In the acute phases, the affected person lives in his delusional world and can hardly be reached. His delusion probably also extends to his relatives, whom he assumes to have threatening intentions and also meets with scepticism.
At the same time, however, the relatives are a very important support for the patient. Their understanding and support are important for the programme of the disease.
As a family member of a schizophrenia patient, you should therefore accept offers of help that inform you in detail about the illness and how to deal with those affected. For example, it is very important that you encourage the person affected to be as independent as possible. In doing so, he or she should neither be underchallenged nor overchallenged. Unique interaction training can serve you additionally.
Also talk to the doctors and therapists treating you and get advice if you are overwhelmed and do not know what to do. Teams of relatives can also be an important help.
FAQ
Below are some frequently asked questions about schizophrenia that people with the condition ask.
Who can you turn to if you have schizophrenia?
If there are signs of severe psychosis, you can consult a professional psychiatric clinic, specialist psychiatrist and psychiatric therapists.
Is schizophrenia psychosis somehow curable?
The disease cannot be cured so far. Nevertheless, it can be treated and – by regulating the signs and avoiding regressions – managed.
How can I deal with paranoid-schizophrenic people?
Keep calm yourself, create a calm, relaxed environment and talk calmly to your relative. Accept if he wants to withdraw. Avoid talking to him or criticising him. Social networks are very important for the person concerned.
How can you get a schizophrenic person to go to the doctor?
The first person to call might be the family doctor. If he thinks it is schizophrenia, he will usually call a specialist in psychiatry and psychiatric therapy. The specialist will talk to the patient to get an idea of their signs and symptoms.
Can one suddenly become ill with schizophrenia?
Schizophrenia can develop imperceptibly and insidiously over years, but it can also start completely unexpectedly with extreme signs and symptoms. After the acute phase has subsided, persistent courses and/or persistent episodes are possible. Relapses occur in about 3 quarters of those affected
What do the imperative voices indicate?
In auditory hallucinations, which are common in people with schizophrenia, the sufferer hears, for example, voices insulting him, commenting on what he is doing, discussing with each other and/or giving orders (critical voices).
What is the course of the disease in schizophrenia?
People with schizophrenia go through a process of acute psychosis – periods when they really see the world differently than they usually do. They may hear voices, feel persecuted or affected by other people. In addition, their behaviour changes and many speak incoherently.
What is the difference between schizophrenia and psychosis?
Psychosis is an umbrella term for a mental disorder in which sufferers lose touch with reality. Most of the time, this disorder is only temporary. Schizophrenia is one of the disorders that can be associated with psychosis. Until today, there is a lot of ignorance and also prejudice among the general public.
What is the difference between schizophrenia and paranoid schizophrenia?
During a stage of paranoid schizophrenia, there is typically no or extremely mild speech disturbances, motor disturbances or apathy – signs and symptoms common to other forms of schizophrenia. People with paranoid schizophrenia also do not show inappropriate or flattened emotions.
How do psychosis and neurosis differ?
In neurosis, there is no known organic cause. Psychosis must be distinguished from neurosis. The difference is the following: The unstable person is aware of his disorder. The psychotic, on the other hand, regards the fact as disturbed – and is not aware of it.
ICD codes for this disorder: F20 | F20.1 | F20.2 | F20.3 | F20.4| F20.5 | F20.6 | F21
ICD codes are internationally valid codes for medical diagnoses. They can be found, for example, in doctors’ letters or on certificates of incapacity for work.
The web content of ÁYIO-Q.com is for your information and in no case replaces a personal consultation or treatment by a qualified physician. The contents of ÁYIO-Q.com cannot and must not be used to make independent diagnoses or for self-medication.
Sources:
- Ramachandran P, Thirunavakarasu P. Vitamins in schizophrenia: a literature review. AP J Psychol Med 2012; 13(2): 74-9, (Vitamine bei Schizophrenie: eine Übersicht der Literatur)
- Firth J, Stubbs B, Sarris J, et al. The effects of vitamin and mineral supplementation on symptoms of schizophrenia: a systematic review and meta-analysis [published correction appears in Psychol Med. 2018 Feb;48(3):528]. Psychol Med. 2017;47(9):1515-1527. doi:10.1017/S0033291717000022
- What is Schizophrenia, Food for the brain Foundation, auf https://foodforthebrain.org/, Zugriff 15.01.2022
- Brown HE, Roffman JL. Vitamin supplementation in the treatment of schizophrenia. CNS Drugs. 2014;28(7):611-622. doi:10.1007/s40263-014-0172-4
- Amminger, G., Schäfer, M., Schlögelhofer, M. et al. Longer-term outcome in the prevention of psychotic disorders by the Vienna omega-3 study. Nat Commun 6, 7934 (2015). https://doi.org/10.1038/ncomms8934
- Schizophrenie – Treatment, National Alliance of Mental Illness, auf https://www.nami.org/, Zugriff 15.01.2022
- Firth, J., Stubbs, B., Sarris, J., Rosenbaum, S., Teasdale, S., Berk, M., & Yung, A. (2017). Die Auswirkungen einer Vitamin- und Mineralstoffergänzung auf die Symptome der Schizophrenie: Eine systematische Überprüfung und Metaanalyse. Psychologische Medizin, 47 (9), 1515-1527. doi:10.1017/S0033291717000022
- The Vitamins in Psychosis Study: A Randomized, Double-Blind, Placebo-Controlled Trial of the Effects of Vitamins B12, B6, and Folic Acid on Symptoms and Neurocognition in First-Episode Psychosis, auf https://www.sciencedirect.com/, zugriff 15.01.2022
- Ramachandran P, Thirunavakarasu P. Vitamins in schizophrenia: a literature review. AP J Psychol Med 2012; 13(2): 74-9, (Vitamins in schizophrenia: a review of the literature).
- Suboticanec, K & Folnegović-Smalc, V & Turcin, R & Mestrović, B & Buzina, R. (1986). Plasma levels and urinary vitamin C excretion in schizophrenic patients. Human nutrition. Clinical nutrition. 40. 421-8.
- Umar MU, Isa AA, Abba AH. High dose pyridoxine for the treatment of tardive dyskinesia: clinical case and review of literature. Ther Adv Psychopharmacol. 2016;6(2):152-156. doi:10.1177/2045125315616738
- Kalaydjian AE, Eaton W, Cascella N, Fasano A. The gluten connection: the association between schizophrenia and celiac disease. Acta Psychiatr Scand. 2006;113(2):82-90. doi:10.1111/j.1600-0447.2005.00687.x
- Kraft, B.D., Westman, E.C. Schizophrenia, gluten, and low-carbohydrate, ketogenic diets: a case report and review of the literature. Nutr Metab (Lond) 6, 10 (2009). https://doi.org/10.1186/1743-7075-6-10
- Deng H, Xu J. Wendan-Abkochung (Traditionelle chinesische Medizin) für Schizophrenie. Cochrane Database of Systematic Reviews 2017, Ausgabe 6. Art.-Nr. Nr.: CD012217. DOI: 10.1002/14651858.CD012217.pub2. Abgerufen am 15. Januar 2022.
- Judson A. Brewer, Patrick D. Worhunsky, Jeremy R. Gray, Yi-Yuan Tang, Jochen Weber, Hedy Kober,Meditation experience is associated with differences in default mode network activity and connectivity, Proceedings of the National Academy of Sciences Dec 2011, 108 (50) 20254-20259; DOI: 10.1073/pnas.1112029108