Updated on 12. April 2022 from ÁYIO-Q Redaktion
Reading time: approx. 15 minutes
Intestinal alarm: When diverticula cause abdominal pain
Diverticulosis is one of the most common human diseases in the western world, affecting up to 50% of the population. Diverticulosis is asymptomatic, i.e. the affected person is symptom-free and does not require any special therapy. Diverticula are extremely common, especially in older people in industrialised countries, and inflammation also occurs in every fourth to fifth person affected. These people then have complaints that are due to the inflammation of a diverticulum, diverticulitis.
Learn here what symptoms it triggers and what role diet plays. Diverticulitis can be successfully stopped: There are reliable therapies in the form of dietary measures and exercise therapy. In this way, the risk of inflammation can be significantly reduced – or even completely eliminated. Without personal effort, however, not much will change. But the initiative is worthwhile, because severe problems considerably limit the quality of life.
- Description
- Shapes & Categories
- Symptoms
- Causes & Risk factors
- frequency
- Progress
- Diagnosis
- Conventional medicine treatment
- Prevention
- Natural & alternative therapies
What kind of disease is diverticulitis?
Whether diverticulosis develops and becomes diverticulitis can be influenced by preventive measures. This is where the great opportunity of naturopathy lies: with the right diet plan and also a lot of exercise, the diagnosis is much more favourable. A permanent change in the diet plan is the simplest known treatment against diverticulitis.
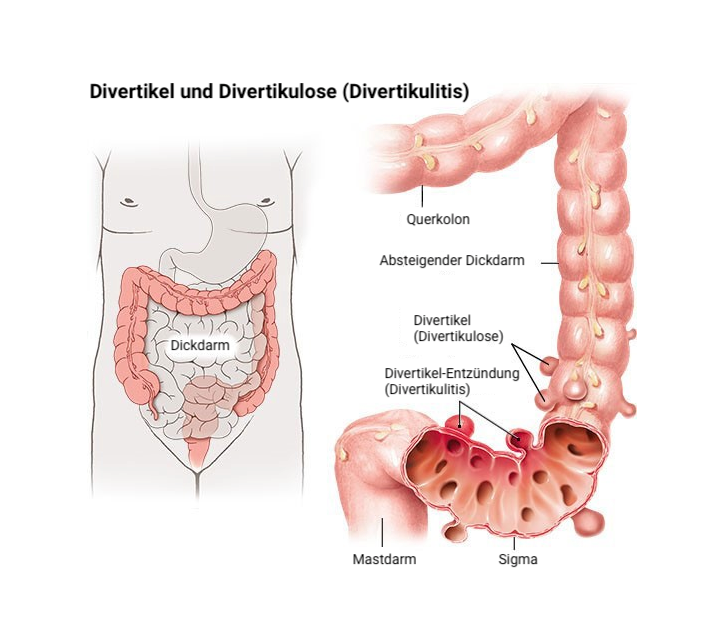
Diverticulitis is a disease in which outpouchings in the small or large intestine become irritated. These protrusions are called diverticula by doctors; if several diverticula are present, it is called diverticulosis. Diverticula of the digestive tract are not in themselves pathological and do not initially cause any symptoms.
In around 90 to 95 % of cases, they develop in the descending branch of the colon, especially at the point where the intestine makes an S-shaped bend (sigmoid). When the diverticula become inflamed, symptoms such as stomach discomfort, high fever, flatulence and irregularity can occur.
One of the suspected causes of diverticulitis is that pathogenic germs colonise the diverticula in addition to the collected stool. Probiotics made from certain yeasts or germs are therefore also worth trying, according to current research studies.
Phytotherapeutics stabilise bowel movements and also minimise the use of medication.
What are the different forms & categories of diverticulitis ?
Doctors distinguish between different forms or stages of diverticulitis:
- In about 75 percent of cases, it is an acute, uncomplicated diverticulitis. In this case, the diverticula may cause unpleasant signs and symptoms, but do not cause any additional problems or damage to the wall surface of the digestive tract. Conventional diverticulitis treatment is usually possible.
- In the case of severe diverticulitis the irritated outpouchings bring further problems, e.g. abscesses, fistulas, intestinal obstruction or a hole (perforation) in the wall surface of the digestive tract. Surgical intervention for diverticulitis is then usually essential to avoid serious health consequences.
- In people with persistent recurrent diverticulitis, the diverticula are repeatedly irritated, causing permanent damage to the wall of the digestive tract. Those affected suffer from persistent pain, constipation and various other symptoms.
The inflammation is usually confined to the area around certain diverticula (peridiverticulitis), but it can also spread to larger areas of the bowel (pericolitis).
Diverticulitis is directly classified into different categories depending on the degree of inflammation:
- Grade 0: only protrusions (diverticulosis)
- Grade 1: Diverticulitis, pain, possibly high fever.
- Grade 2: acute, difficult diverticulitis: inflammation of the diverticulum and the adjacent cells, possibly purulent, possibly opening.
- Grade 3: persistent: recurrent swelling.
A distinction is made depending on the manifestation:
- True diverticula: They are hereditary. All layers are involved, consisting of the muscular layer of the intestine.
- Non-genuine diverticula: They do not involve all the layers of the intestinal tract: Only the mucous membrane of the digestive tract protrudes outwards, with a space in between in the muscle tissue. When faeces are trapped in the diverticulum, there is no muscle tissue to carry them back into the intestine.
What are the symptoms of diverticulitis?
Diverticulitis can trigger various signs. These can occur in varying degrees of intensity. In acute diverticulitis, the following signs predominate:
- Pain that occurs unexpectedly, persists and generally affects the left lower abdominal area. However, they can also occur on the right side, in the middle or in the lower abdominal area. Generally, the pain increases with food intake and improves after bowel movements or defecation. The discomfort may also increase with physical activity. In addition, they may radiate to other parts of the body.
- Fever
- Solidified structures (“roller”) in the abdominal area associated with inflammation
- Strong feeling of illness
- Stool irregularities such as constipation (in addition, lambskin-like stools are possible), diarrhoea and flatulence.
- Excretory stimulus, which can be extremely distressing
- Nausea or vomiting
- Loss of appetite
Possible signs of chronic diverticulitis
Chronic diverticulitis can lead to complications and can be manifested by the following signs and symptoms:
- Blood in the stool (diverticular bleeding)
- Bleeding from the anus (rectal blood loss)
- Narrowing of the digestive tract (stenosis) up to digestive congestion (ileus)
- Breakthrough of the intestine (perforation)
- Peritonitis ( inflammation of the peritoneum)
- Abscesses – encapsulated collections of pus
- Fistulas – channel-like connecting ducts between the swollen diverticulum and various other bowel sections or adjacent body organs. If the urinary bladder is affected, cystitis may occur. If the vagina is affected, there may be discomfort in the genital area (also during sexual intercourse).
- Detectable blood in the urine
What causes and risk factors can trigger diverticulitis?
The causes of diverticulitis can be manifold. Diet plays an important role. A diet low in fibre increases the occurrence of diverticula in the digestive tract. According to the German Society for Gastroenterology, Digestive and Metabolic Diseases (DGVS), it is the “most important risk variable for diverticular disease”.
In people prone to diverticulosis, very high pressure has been measured in the colon. This stretches the wall surface of the digestive tract with ” no resilience ” until eventually a small sac forms. At risk are therefore places or patches where blood vessels pass through the muscular layer of the intestine.
The following explains the connection between diet, dietary fibre and diverticulitis:
1. Foods rich in fibre
Dietary fibre binds water in the digestive tract. This makes the faeces softer and also more voluminous. It can then be transported through the digestive tract more easily and also exerts less pressure on the intestinal wall.
2. Low-fibre foods
Low-fibre foods, on the other hand, cause the stool to become firm and also hard. The intestinal muscles have to exert even more pressure to move the stool through the digestive tract. If stool with microorganisms accumulates there, diverticulitis can develop.
The fact that nutrition plays a special role in diverticular disease is also reflected in the historical development: Since about 100 years, the number of diverticulitis patients in western industrialised countries has increased sharply, parallel to the adjustment of many people’s eating habits.
Today, this usually looks like this:
- Fruit, vegetables and wholemeal products, which are rich in fibre, are hardly ever found on the plate at home.
- Pizza, French fries, burgers or various other convenience foods that contain hardly any fibre are typically on the menu instead.
- High meat consumption is also considered a risk aspect for the development of diverticula in the digestive tract. Especially the increased consumption of red meat, such as pork, lamb, beef or veal, has greatly increased.
Diverticulitis: Are there other causes?
There are other known risk factors that increase the risk of diverticulitis. These consist of, for example:
- Age: For many people, connective tissue weakens with age. Diverticula occur in 1 in 10 people over 50 and in 1 in 3 over 60. Of those over 70, more than 60 per cent have such benign changes in the bowel. Younger people may also have less flexible connective tissue. The predisposition to this can be hereditary
- Overweight: (typically a result of poor diet) and lack of exercise – low physical activity also affects bowel function.
- Painkillers: Constant use of painkillers from the group of non-steroidal anti-inflammatory drugs (NSAIDs) can promote swelling of the intestines. The active substances from this group include ibuprofen, diclofenac and also acetylsalicylic acid (ASA).
Frequency of diverticulitis
Many people have diverticulosis without knowing it. Diverticula become more typical with age: about 10% of people under 50 have diverticula, and about 50% of people over 70. They occur with similar regularity in women and men.
Diverticulitis develops in about 1 % of all people with diverticulosis within ten years. The inflammation can occur at any age.
Course of diverticulitis
Diverticulosis itself is relatively harmless. It is usually an uncomplicated diverticulitis that also resolves itself under conventional therapy with dietary measures, optimisation of risk factors and possibly the administration of prescription antibiotics.
When digestive components get stuck in the diverticula, they solidify and supposed lumps of faeces form. The mucous membrane, which is completely under pressure, is less well nourished and supplied with blood, so that inflammation and blood loss often occur. In some cases, microorganisms also collect in the diverticula and pus also forms.
An attack is followed by a symptom-free period. With an ideal lifestyle, sufferers can be permanently healthy and balanced. Research has shown that many sufferers do not implement the suggestions effectively. As a rule, 30 % of those affected suffer a relapse.
How is diverticulitis diagnosed?
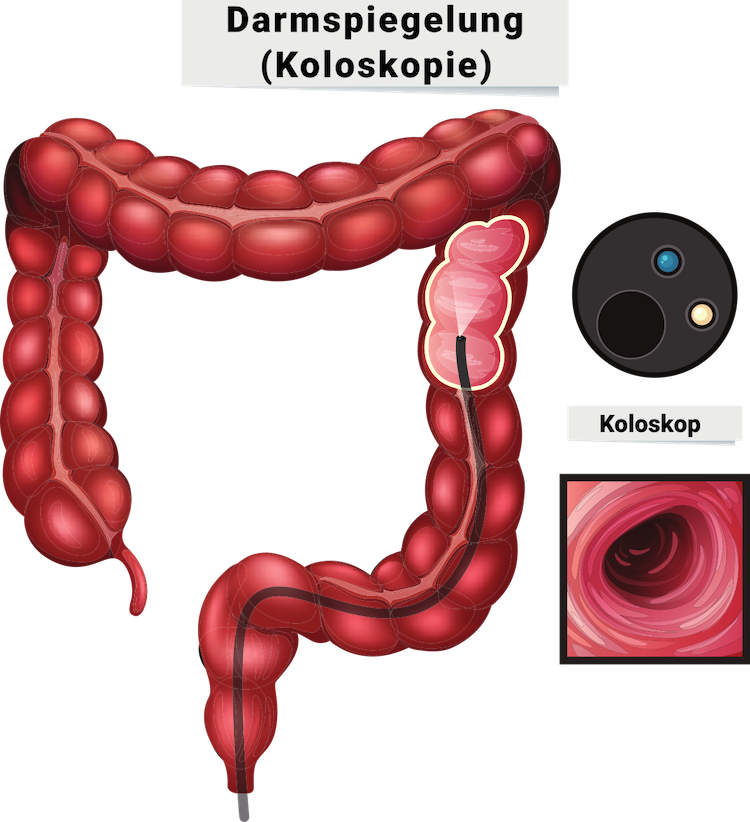
The doctor obtains decisive information for the medical diagnosis of diverticulitis from the patient’s medical history. He asks the patient where exactly the pain is located and how it feels. Other points such as fever and bowel irregularities are also important clues, as is the question of whether such an event has occurred before. Some people know they have diverticula in their bowel or have already gone through diverticulitis. It is not uncommon for doctors to discover diverticula by chance during a colonoscopy.
In severe diverticulitis, a colonoscopy would be too risky. It is often suggested that the examination be carried out about 4 to 6 weeks after the diverticulitis has healed. The aim is to check whether the signs and symptoms are not caused by polyps, colon cancer cells or various other diseases.
Sometimes doctors can feel the swollen diverticula as a hard framework in the left lower abdomen. Palpation can be painful in diverticulitis. The physical examination additionally consists of the doctor palpating the rectum with his finger to detect changes in the rectum (digital-rectal examination).
Blood tests often show increased levels of inflammation in diverticulitis – for example, an increased number of white blood cells (leukocytes), an altered erythrocyte sedimentation rate (ESR) and an increased C-reactive protein (CRP). A trained examiner can also detect the swollen diverticula on ultrasound. However, with the help of computed tomography (CT) or magnetic resonance imaging (MRI), diverticulitis can be detected much more precisely.
In some cases, an X-ray of the abdomen in a standing position is necessary to detect diverticulitis: When a diverticulum ruptures, additional air can enter the abdomen, which accumulates under the diaphragm and is also clearly visible on the X-ray.
What are the conventional medical treatment options for diverticulitis?
New-onset, uncomplicated diverticulitis is treated conservatively; conservative therapy is also recommended for new-onset diverticular bleeding, depending on the severity. The therapy for diverticulitis consists of dietary restriction or a low-fibre diet plan, taking medication for the symptoms and treatment with antibiotics. In the case of moderate signs and symptoms without complications, this treatment can additionally be carried out on an outpatient basis if the affected person tolerates this well.
Diverticular bleeding is usually a complication of non-inflammatory diverticulosis, but can also occur in diverticulitis. It can be treated well in 90 % of cases and usually also subsides spontaneously. Otherwise, a picture of the bleeding site is taken during a colonoscopy (endoscopy).
In the case of recurrent inflammation with changes in the intestine (e.g. narrowing or incipient blockages), drug therapy with removal of the affected section of the intestine is necessary. In high-risk patients and in patients under 40 years of age, surgery should be performed after the first inflammatory episode because of the high risk of recurrence. In case of a hidden perforation, resection is performed immediately or after appropriate treatment during the inflammation-free period.
Today, there is every reason to believe that antibiotics and surgery are less necessary than previously thought.
What surgical procedures are available?

Due to advances in medical therapy, the removal of the diverticulum-bearing part of the intestinal tract, similar to the removal of the gallbladder, can now be performed minimally invasively – laparoscopically – for most people. For those affected, this means a much shorter inpatient stay, much less scarring, much less discomfort and less scarring.
The laparoscopic resection of the diverticulum-bearing bowel segment is performed with 4 to 5 tiny incisions in the skin, and the digestive tract is also sutured back together without an artificial exit. Usually, a plastic tube is inserted through one of these skin incisions to drain the injury secretion, which is removed after a few days.
In an emergency situation (free bowel rupture, peritoneal surgical treatment, bowel obstruction), there is always a need (sign) for surgical intervention. In these situations, surgery via an abdominal incision is almost always necessary. As a rule, an artificial anus is created for a short time in this situation, but it can be returned after some time. Moreover, in such a case there is an acute danger to life, so that especially in the case of recurrent diverticulitis, a possible operation must be considered in good time.
What preventive measures are useful?
You cannot stop the age-related decline in connective tissue strength, but you do have it in your hands to eat healthy and exercise. Both are essential factors, not only in the fight against diverticulitis, but also in its prevention.
Some dietary advice discourages certain foods, especially nuts, grains, corn and snacks. For a long time it was thought that small deposits of these foods get stuck in the diverticula and promote swelling.
You can therefore do a lot yourself to prevent diverticulitis from developing (again).
The following measures are useful for this purpose:
- Make sure you eat a high-fibre diet with lots of vegetables, fruit and wholemeal products.
- Drink enough – about 1.5 to 2 litres daily
- Do not smoke
- Avoid being overweight or obese (obesity)
- Regular exercise improves the digestion of food. Get at least 30 minutes of exercise a day. Go for a brisk walk often and also do sport a few times a week, e.g. running, swimming or dancing.
23 tips for natural therapies for diverticulitis
Acute diverticulitis and also its complications are treated according to their intensity. In mild cases, physical rest and a change to a liquid diet (e.g. tea with glucose and clear broth) are sufficient to calm the process. Sometimes laxatives also help.
In the past, antibiotics were usually prescribed for suspected diverticulitis without further medical diagnosis. Nowadays, however, people are less and less willing to administer antibiotics because they also reduce the beneficial microorganisms in the digestive tract and disturb the natural balance of the microbiome in the digestive tract. This can actually do more harm than good.
Do you have problems with diverticulitis? If so, you are not alone. Diverticulitis is a nagging problem that is unfortunately becoming more common in developed countries due to increasingly harmful lifestyles. In addition to lifestyle changes, there are many natural, herbal solutions you can use to help heal your gastrointestinal system and prevent further damage.
Medicinal plants against diverticulitis
1. Wheat bran, oat bran
These fibres swell and additionally expand the intestine. This increases the tension in the wall of the digestive tract, which minimises the formation of diverticula. The size should be as coarse as possible (at least 1 mm). However, the microorganisms in the intestine also absorb these compounds, so some people get unwanted flatulence – much less bad than diverticulitis, but just as unpleasant.
2. Psyllium and linseed
The pods of these seeds absorb large amounts of water. Mucilages are formed that have both anti-inflammatory and soothing effects, making them suitable for the long-term treatment of uncomplicated diverticulitis, especially when the diverticulitis subsides after fasting. In the medical studies, both the granules of the seeds and the seed coats were used (2 teaspoons before the morning meal as well as after dinner, daily dose 20 g).
3. Oregano
The medicinal plant oregano is well suited for complaints of the entire digestive system, e.g. by preparing a tea for internal use from a teaspoon of the dried natural herb and 250 ml of boiling water and letting it steep for about 5 minutes.
4. Turmeric
Turmeric longa is one of the traditional herbal medicines. Among other things, it contains starch, sugars, the necessary oil to stimulate bile production in the liver, and the active ingredient curcumin, which makes the plant so healthy and balanced. Curcumin is a yellow pigment and is also just one of the curcuminoids (fat-soluble second plant substances) that can be extracted from the root of the Curcuma longage plant. The substance is said to have the following properties, to name but a few:
- anti-inflammatory
- antioxidant
- antiviral
- antibacterial
- bile-promoting
The body particularly benefits from the latter effect because: Turmeric extract can help increase the flow of bile and thus also relieve signs and symptoms of acid indigestion such as unwanted flatulence. Various other uses include mild bile-liver problems – for example, a practical disorder – as well as shortness of breath and an irritated bowel.
5. Caraway
As a fragrant natural herb, caraway is not only ideal for cooking. It also acts as a “caretaker” for the body. Full of healthy proteins, oils and minerals and vitamins, it can be used for a range of digestive complaints, including irregular bowel movements, colic, flatulence, acid indigestion, heartburn, pain and irritable bowel syndrome. It can speed up gastrointestinal processes and also stimulate cravings. It also aids digestion and can protect your digestive system from infections associated with abscesses and IBS. The dietary fibre in caraway additionally binds toxins in food and protects the colon from cancer cells. Herbalists consider it one of the best supplements for improving the digestive tract. When combined with fennel and peppermint, it works even more efficiently.
6. marjoram
Related to oregano, marjoram is an herbal plant. It is good for digestion and also relieves an acid stomach and also eliminates stomach discomfort. It shares the antifungal and anti-inflammatory properties of oregano, but is more peaceful, so it is much better at helping to relax your nerves and remove tension.
7. Aloe vera juice
When used frequently, aloe vera is effective in curing gastrointestinal problems such as diverticulitis. The majority of users report that the effect occurs after 3 to 30 days, depending on the intensity of the problem. It can also be used as a base for castings to combat an unpleasant or strong taste. If desired, any type of citrus-free juice can also be added for flavour.
8. Barley grass
Barley is one of the first grains to be cultivated and is a true nutritional giant. It can help with detoxification, internal cleansing and also cell fixation and also provides practically 30+ minerals and vitamins that are important for human health. Due to its natural cleansing properties, it is highly recommended for heavy metal poisoning as it binds to metals such as lead, mercury and aluminium and transports them out of the body. In addition, it can help to resolve inflammation as well as eliminate damaged cells in the digestive system.
As a digestive aid, it can help relieve indigestion, heartburn, unwanted flatulence, nausea or vomiting, gastritis, gastric and duodenal abscesses and increase appetite. As it promotes digestive health and also helps with daily balance, it can additionally help prevent and treat diverticulitis.
Barley grass is available in both powder and pill form. Simply take the dosage recommended by the supplier.
9. Kelp
Kelp as well as various other seaweeds are rich in nutrients and contain normally occurring iodine. Herbalists claim that salt alginate, the energetic component in kelp, binds it in the gastrointestinal system.
Kelp also promotes the health and well-being of the thyroid, adrenal and pituitary glands and relaxes a disturbed gastrointestinal system. It helps with irregularities in bowel movements and flatulence.
As a source of over 70 trace elements and many important vitamins and minerals, seaweed is a basic tonic. Not only does it help remove waste from the body more easily, it also helps balance pH levels, improve overall food digestion and kidney function, and purify the blood.
10. Extract of papaya leaves
Papaya leaf extract can help because it contains papain. This is an enzyme that helps the body break down both proteins and carbohydrates. It also helps with constipation and contains minerals, B vitamins and vitamin C.
11. Grapefruit seed extract
Additionally, because it is alkalising, grapefruit seed extract helps to balance your internal pH. It not only fights diverticulitis, but also improves the intestinal flora so that your body can heal by helping to restore the balance of your intestinal flora.
12. Wild yam
Wild yam is rich in plant hormones and can be used to balance hormones. It is an antispasmodic and is used to eliminate abdominal pain and irritable bowel syndrome (IBS) as well as ovarian and uterine pain and various other cramps.
13. Liquorice
Licorice supports food digestion and the health and well-being of the gut. It can line the cell walls of the abdomen with mucus and soothe the mucous membranes that protect the digestive system.
14. Marigold
The marigold, also called calendula, has been used for hundreds of years in the form of infusions. It is an excellent medicinal plant for colitis, acid indigestion, heartburn, abdominal cramps and also for intestinal sluggishness. Calendula inhibits the formation of microorganisms that cause stomach ulcers and gastritis, thus helping to protect your stomach and intestinal mucosa.
15. Cat’s claw
Since its discovery in the Peruvian rainforest, cat’s claw has become widely known as an immune stimulant. It has antiviral and anti-inflammatory properties and is rich in antioxidants. It is considered a “life-giving” tonic and has a wide range of restorative uses, but is especially helpful for supporting the digestive system. It helps to cleanse the digestive tract, balance the intestinal flora and strengthen the immune system.
16. Elm bark (slippery elm)
Slippery elm bark relieves inflammation in the digestive tract. One of its oldest uses was as a tonic for the digestive tract. Its high mucilage content eliminates stomach inflammation and neutralises excess stomach acid, making it an excellent solution for the digestive tract. It was also used to relieve constipation and persistent constipation.
17. Quercetin and rutin: flavonoids with anti-inflammatory effects in the digestive tract
Mode of action of quercetin and rutin
Both quercetin and rutin are plant substances. They come from the flavonoid group and reduce the formation of inflammatory messenger substances. In addition, they scavenge free oxygen radicals and thus protect the body’s cells from damaging inflammatory reactions (oxidative stress and anxiety). Since inflammation of the diverticula must be avoided in diverticulosis, quercetin and rutin could protect against the signs.
Studies from domestic animal research suggest that rutin may help with inflammatory diseases of the gut. There are already studies on quercetin in humans: an initial examination of a series of high-quality research studies shows that quercetin minimises inflammation levels in the blood. Animal and laboratory studies have also shown that the plant compound alleviates inflammatory diseases in the colon.
Whether quercetin and rutin actually help with diverticulosis and inflamed diverticula cannot yet be said with certainty. In any case, a plant-based diet with lots of vegetables and fruit is recommended: It is not only rich in quercetin, rutin and various other flavonoids, but also contains a lot of dietary fibre.
Dosage and recommended intake of quercetin and rutin
Overall, it has been shown that a dietary plan with 300 milligrams of flavonoids per day is helpful for the health of the digestive tract. Accordingly, preparations can be supplemented on a trial basis – for example, 150 milligrams of rutin and also 150 milligrams of quercetin. The preparations must be taken together with a meal.
To be observed during pregnancy, breastfeeding, in case of illness and when taking medication;
Quercetin should not be taken during pregnancy or while breast-feeding: Sufficient studies are not available. The intake of rutin, on the other hand, should be discussed with a doctor. Studies are available on some areas of application (e.g. haemorrhoids).
Patients with liver disease or kidney weakness (renal deficiency) cannot completely excrete both rutin and quercetin. In these cases, you should only take rutin and also quercetin after consulting your doctor. People who suffer from water retention due to heart disease should not take rutin.
Diet for diverticulitis
18. Diet plan in liquid form
A specialist therapist may recommend a temporary liquid diet to a person suffering from a flare-up of symptoms. Foods and drinks that the person can prepare at home include:
- Water, tea and coffee without milk
- strained fruit juices without pulp, such as white grape or apple juice
- Chicken or beef broth
- Popsicles without pulp or other ingredients
- Jelly without fruit
Sufferers only need to follow the liquid diet for as long as their specialist therapist recommends. This ensures that they do not have to miss out on necessary nutrients.
When the signs subside, the doctor will certainly advise gradually reintroducing stronger foods into the diet.
19. First follow a low-fibre diet
A diet low in fibre can further alleviate the symptoms of diverticulitis.
Low-fibre foods include:
- Cooked fruit or canned fruit without seeds or peels
- Well-cooked vegetables without seeds or peelings
- Eggs
- Dairy products
- White bread
- white noodles
- White rice
- Well cooked or ground meat
- low-fibre grains
The signs usually improve within 2-4 days, after which you can try slowly adding small amounts of fibre again.
20. Slowly increase the consumption of dietary fibre
As long as the signs do not flare up again, experts advise that diverticulitis sufferers include fibre in their diet.
Fibre can protect against irregularity in bowel movements. If a person has to strain a lot to have a bowel movement, this can cause the colon to bulge, which increases the likelihood of a hernia (hernia sac) forming.
It is also very important to drink enough water to make bowel movements soft and easy to manage.
Some high-fibre foods are:
- Vegetables, including potatoes, green peas, cabbage and pumpkin
- Fruit, including apples, pears, avocados and also bananas
- Cereals, including wholemeal bread, pasta, rice, quinoa and barley
- High-fibre grains consisting of bran and oats
- Beans and pulses, consisting of chickpeas, lentils, kidney beans and peas
21. Protection and strengthening of the mucous membranes of the digestive tract by probiotics
Mode of action of probiotics
Probiotics are living bacteria (primarily germs) with health-promoting properties. They are very important for a healthy and balanced intestinal flora and also displace harmful bacteria in the intestinal tract. An accumulation of disease-causing microorganisms is probably associated with diverticulitis. If needed, taking probiotics could protect against the symptoms caused by diverticulosis.
Several studies have found that probiotics reduce the risk of diverticulitis. This is shown in various review articles. The researchers assume that at least 6 out of 10 people benefit from taking probiotics: They had fewer complaints. Furthermore, the risk for additional diseases was minimised – for example, for narrowings in the intestinal tract (stenoses). Microorganisms of the genus “Lactobacillus” were used most frequently. The probiotics were studied in patients who suffered from diverticulosis, diverticulitis or frequent relapses.
A clear verdict on probiotics in the treatment of diverticulosis is not yet possible. Since numerous initial research studies provide positive results, taking probiotics is worth a try.
Dose and recommended intake of probiotics
Nutritionists advise that probiotics should always be taken in sufficient quantities and also on a normal basis: This is the only way to get enough living bacteria into the intestinal tract. This requires 1 to 20 billion bacteria (1 to 20 x 109) per day. The following types of microorganisms have been shown to be helpful in diverticular diseases:
- Lactobacillus cacidophilus
- Lactobacillus plantarum
- Lactobacillus paracasei
- Lactobacillus delbrueckii subsp. bulgaris
- Lactobacillus casei subsp. DG.
The preparations are offered in capsule form or as powder to be stirred into water or food such as yoghurt. The preparation should contain as many different types of bacteria as possible: This makes the germs particularly resistant and increases the likelihood that they will reach the intestinal tract at all.
Vitamins for diverticulitis
22. Vitamin D
Some studies suggest that people with reduced vitamin D levels have an increased risk of diverticulitis and its associated problems. However, scientists have not yet been able to confirm this conclusively.
Some dietary sources of vitamin D are:
- fatty fish, such as tuna, salmon and mackerel
- Beef liver
- Eggs
- Cheese
- some mushrooms, including those grown under UV light
- starchy foods, such as breakfast cereals, vegetable milk and margarine
- Direct sunlight exposure
Many people meet their daily requirement of vitamin D through direct exposure to sunlight. UV light converts compounds in the skin directly into vitamin D.
The liver and fat cells also store vitamin D to use at a later time when light conditions are worse.
Sunlight helps the body to produce vitamin D. Nevertheless, people need to protect themselves from sunlight damage by using sunscreen and avoiding UV radiation from sunbeds.
Food supplements
Individuals can also take vitamin D as a food supplement to replenish their vitamin D levels. This can be helpful when light levels are reduced during cold weather. It can also help people who do not eat many foods rich in vitamin D.
Vitamin D preparations come in two varieties: D-2 (ergocalciferol) and also D-3 (cholecalciferol). According to the National Institutes of Health (NIH), vitamin D-2 can be less effective than D-3 in higher doses.
Minerals for diverticulitis
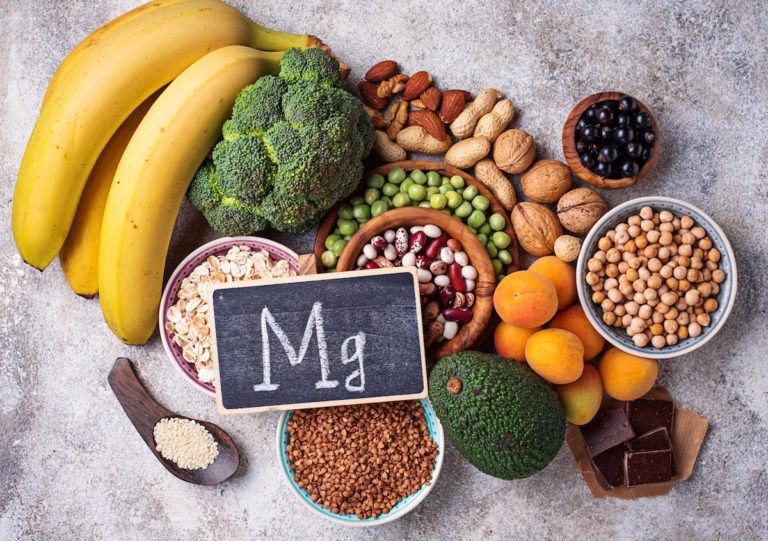
23. Magnesium
Mode of action of magnesium
Magnesium softens hard stools and has a mild laxative effect: it “pulls” water back into the intestine (osmotic effect) and stimulates the muscles in the intestine. A soft bowel movement not only makes it easier to go to the toilet, but can also prevent the development of new diverticula. Diverticula are most likely to develop if the stool is pushed out too much.
However, for constipation, magnesium is one of the typically approved treatments in micronutrient medicine. Magnesium could therefore also be beneficial in the treatment and prevention of diverticulosis.
Dosage and recommended intake of magnesium
For the therapy of diverticulosis, micronutrient experts recommend a supplementation of 300 to 600 milligrams of magnesium. However, if quantities above 250 milligrams are taken in full, this must be discussed with the doctor. For quick relief of bowel irregularities, a single dose of 1,200 milligrams is recommended. For irregular bowel movements, the compound magnesium oxide is best.
The response to magnesium sometimes varies. It is therefore recommended to start with a low dose – for example 300 milligrams – and to spread the whole dose over the day.
The tip at the end
Our world is increasingly toxic. When we get sick, we are often prescribed a pill that can have unwanted negative effects and only treats the symptoms without addressing the underlying causes. It is time to pay less attention to the pharmaceutical-industrial complex and discover herbal treatments that offer a mild, holistic treatment and address the underlying causes in addition to the signs and symptoms.
Especially with conditions like diverticulitis, which are becoming increasingly difficult to treat and can significantly affect quality of life, it is important to take responsibility for self-care. As always, you need to discuss these natural remedies with your doctor and together create a sustainable plan to help your body regain vitality and integrity.
FAQ
Below are some frequently asked questions about diverticulitis that sufferers ask.
What can I do against diverticulitis?
The treatment of severe diverticulitis and its problems depends on its severity. In mild courses, physical rest and a change to a liquid diet (e.g. tea with sugar and also clear broth) are sufficient to relax the process. Often, laxative measures also help.
Does heat help with diverticulitis?
Uncomplicated diverticulitis can usually be relieved with simple steps and natural remedies, such as: Eating only liquid food for a few days and drinking plenty of fluids – this relieves the intestinal tract. Cold or heat are proven home remedies for the symptoms.
For how long should I follow a light diet for diverticulitis?
It is usually recommended that no food is eaten during the first few days of severe diverticulitis and that solid food is only reintroduced gradually (also called food restriction). A one-time sparing diet is suitable for this.
How much should I drink if I have diverticulitis?
Consume at least 1.5 to 2 litres daily! Especially tea (green or organic) and still water (magnesium content > 100 mg/l). This is because dietary fibres bind a lot of water and swell up in the intestines – there is a risk of irregular bowel movements. Probiotics such as Lactobacillus casei to support the intestinal plants seem to have a beneficial effect.
What increases the risk of diverticulitis?
Constant consumption of red meat, e.g. in the form of sausage, can promote diverticulitis. Alternatively, meat can be replaced by fatty fish (rich in omega-3 fatty acids), which, unlike meat, has an anti-inflammatory effect. Sugar: It promotes inflammatory processes.
Can diverticulitis be treated without antibiotics?
In the case of uncomplicated diverticulitis, antibiotics can be dispensed with. The prerequisite for this is that an ultrasound or computer tomography examination has been performed and no abscesses are visible. The medication then most likely does not reduce the risk of complications.
What does the intestine have to do with the subconscious?
The gut interacts greatly with the psyche. It influences the subconscious more than the other way round. It regulates whether we have an appetite or are full, it can increase discovery and influence the state of mind, it can create cravings – a strong desire – as well as addictive habits.
Can the gut trigger anxiety?
The microorganisms in your digestive tract have a major impact on your subconscious – a recent study shows. In the fairly recent microbiome study, evidence is mounting that disturbed gut vegetation can contribute to anxiety and clinical depression.
Which microorganisms of the digestive tract help with depression?
A research paper on this topic was published in the journal Nature Micobiology in February 2019. The researchers found that microbial species of the Coprococcus category, as well as Dialister, were found in reduced amounts in the faeces of people with depression.
How is the gut connected to the brain?
The intestine has its own nervous system, the enteric nervous system, or ENS for short. This ENS runs through the entire gastrointestinal tract and also contains over 100 million nerve cells, more than in our spinal cord. Information is regularly exchanged between the ENS and also the brain.
ICD codes for this condition: K57 | K57.0 | K57.1 | K57.2 | K57.3 | K57.4 | K57.5 | K57.8 | K57.9
ICD codes are internationally valid codes for medical diagnoses. They can be found, for example, in doctors’ letters or on certificates of incapacity for work.
The web content of ÁYIO-Q.com is for your information and in no case replaces a personal consultation or treatment by a qualified physician. The contents of ÁYIO-Q.com cannot and must not be used to make independent diagnoses or for self-medication.
Sources:
- Marinella MA, Mustafa M. Acute diverticulitis in patients aged 40 years and younger. The American Journal of Emergency Medicine . March 2000.
- Balk EM, Adam GP, Cao W et al. Management of Colonic Diverticulitis. (AHRQ Comparative Effectiveness Reviews; No. 233). 2020.
- Lahner E, Bellisario C, Hassan C et al. Probiotics in the Treatment of Diverticular Disease. A Systematic Review. J Gastrointestin Liver Dis 2016; 25(1): 79-86.
- German Society for Gastroenterology, Digestive and Metabolic Diseases (DGVS): First guideline on diverticular disease published: Dietary fibre protects against inflammation of the intestinal mucosa; October 2021, accessed 15.01.2022
- Divertikelkrankheit des Dickdarms. Harvard Health Publishing . 29. August 2020.
- National Health Service UK: Diverticular disease and diverticulitis, auf nhs.uk, Zugriff15.01.2022
- Rezapour M, Ali S, Stollman N. Diverticular Disease: An Update on Pathogenesis and Management. Gut Liver. 2018;12(2):125-132. doi:10.5009/gnl16552
- Vitamin D: Fact sheet for health professionals. (2020), auf https://www.medicalnewstoday.com/, Zugriff 15.01.2022
- Rezapour M, Ali S, Stollman N. Diverticular Disease: An Update on Pathogenesis and Management. Gut Liver. 2018;12(2):125-132. doi:10.5009/gnl16552
- Edith Lahner, Cristina Bellisario, Cesare Hassan, Angelo Zullo, Gianluca Esposito, Bruno Annibale, Probiotics in the Treatment of Diverticular Disease. A Systematic Review, Available from: www.jgld.ro/wp/y2016/n1/a12DOI: http://dx.doi.org/10.15403/jgld.2014.1121.251.srw
- Habtemariam S, Belai A. Natural Therapies of the Inflammatory Bowel Disease: The Case of Rutin and its Aglycone, Quercetin. Mini Rev Med Chem. 2018;18(3):234-243. doi:10.2174/1389557517666170120152417
- Hanai H, Iida T, Takeuchi K, et al. Curcumin maintenance therapy for ulcerative colitis: randomized, multicenter, double-blind, placebo-controlled trial. Clin Gastroenterol Hepatol. 2006;4(12):1502-1506. doi:10.1016/j.cgh.2006.08.008
- Izzo AA, Gaginella TS, Capasso F. The osmotic and intrinsic mechanisms of the pharmacological laxative action of oral high doses of magnesium sulphate. Importance of the release of digestive polypeptides and nitric oxide. Magnes Res. 1996;9(2):133-138.
- Ju S, Ge Y, Li P, et al. Dietary quercetin ameliorates experimental colitis in mouse by remodeling the function of colonic macrophages via a heme oxygenase-1-dependent pathway. Cell Cycle. 2018;17(1):53-63. doi:10.1080/15384101.2017.1387701
- Kwon KH, Murakami A, Tanaka T, Ohigashi H. Dietary rutin, but not its aglycone quercetin, ameliorates dextran sulfate sodium-induced experimental colitis in mice: attenuation of pro-inflammatory gene expression. Biochem Pharmacol. 2005;69(3):395-406. doi:10.1016/j.bcp.2004.10.015
- Tursi A, Elisei W, Picchio M, Di Mario F, Brandimarte G. Serum levels of vitamin D are associated with the severity of the endoscopic appearance of diverticular disease of the colon according to DICA classification. J Gastrointestin Liver Dis. 2016;25(4):567-568.
- A systematic review of high-fibre dietary therapy in diverticular disease, auf https://link.springer.com/, Zugriff 15.01.2022