Updated on 12. April 2022 from ÁYIO-Q Redaktion
Reading time: approx. 15 minutes
Ulcerative colitis – The enemy hides in your own body
Together with Crohn’s disease, ulcerative colitis is one of the most common chronic inflammatory diseases of the colon (IBD). The disease is most common in industrialised countries and especially in the urban population.
In Europe, the incidence of ulcerative colitis varies between 1 and 58 new cases per 100,000 inhabitants. There is a north-south gradient with a cluster of cases in Scandinavia.
In Germany and France, the incidence is 3 to 5 per 100,000 inhabitants per year. White people have a four times higher risk of contracting the disease than people with other skin colours.
A common sign and symptom is diarrhoea with blood and mucus admixtures. Ulcerative colitis usually progresses in episodes: During the symptom-free period, normal everyday life is possible.
Have you been diagnosed with ulcerative colitis? Read here how you can help yourself with ulcerative colitis, how the diet plan affects the disease and exactly how the inflammation of the colon works.
- Description
- Forms
- Symptoms
- Causes & Risk factors
- Diagnosis
- Conventional treatment
- Course of the disease & prognosis
- Natural & alternative therapies
Ulcerative colitis – What is it ?
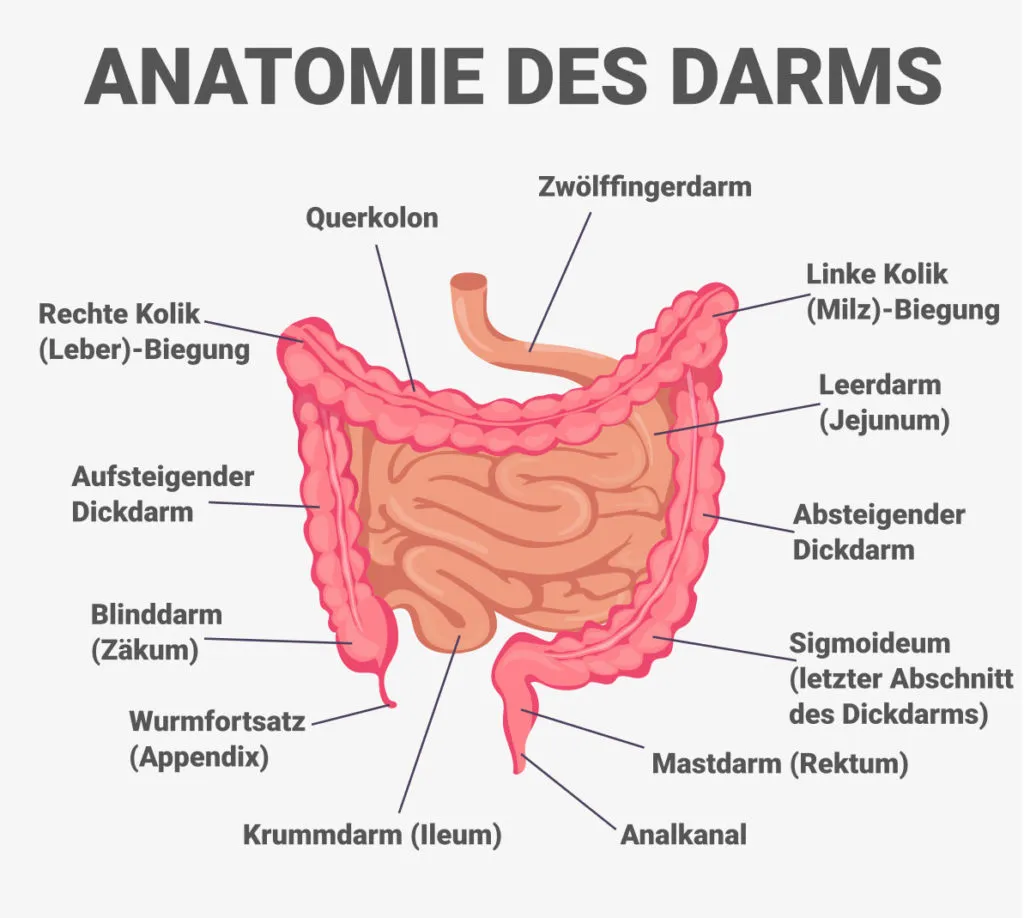
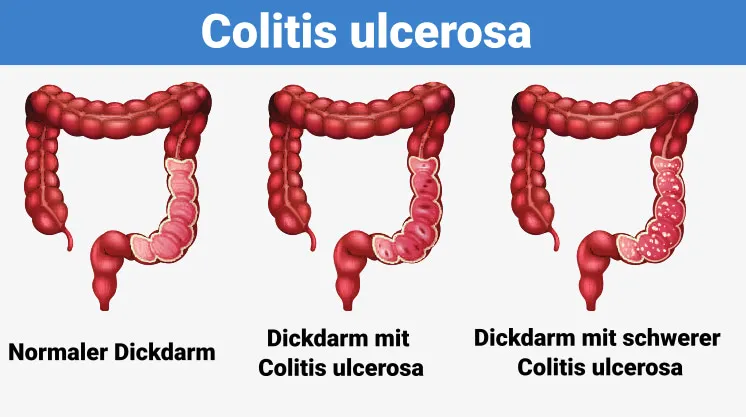
Ulcerative colitis occurs when the cell walls of the large intestine (also called the colon), the anus or both become inflamed. This inflammation leads to tiny ulcers on the lining of the intestine called ulcerative colitis. The inflammation typically starts in the rectum and spreads upwards. It can affect the entire colon.
Inflammation makes your digestive tract move its components quickly and also empty them frequently. When cells on the surface of the intestinal mucosa become detached, ulcers can form. The abscess can lead to bleeding and the discharge of mucus and pus.
Although this disease affects people of all ages, according to the American Gastroenterological Organization, many people develop ulcerative colitis between the ages of 15 and 30. From the age of 50, there is an additional small increase in the diagnosis of IBD, generally in men.
Forms of ulcerative colitis ?
Ulcerative colitis can be classified according to the parts of the gastrointestinal tract that it affects:
- Ulcerative proctitis: In ulcerative Proctitis only the anus is inflamed. It is considered a moderate form of ulcerative colitis.
- Left-sided colitis: Left-sided colitis is additionally known as distal ulcerative colitis.
- Proctosigmoiditis: Proctosigmoiditis is a form of left-sided colitis. It causes swelling in the anus and sigmoid colon.
- Pancolitis: Extensive colitis, also called pancolitis, causes inflammation throughout the colon. It is considered a severe form of ulcerative colitis.
What are the symptoms of ulcerative colitis ?
The severity of the signs of ulcerative colitis varies depending on the person who has the disease. Symptoms may also change over time.
People diagnosed with ulcerative colitis may experience periods of mild signs and symptoms or no symptoms at all. Symptoms may return and become extreme.
Common symptoms of ulcerative colitis include:
- Abdominal discomfort
- increased abdominal sounds
- bloody stool
- Diarrhoea
- Fever
- rectal discomfort
- weight loss
- Malnutrition
Ulcerative colitis can cause additional signs and symptoms, such as:
- Joint complaints
- Joint inflammation
- Nausea and reduced appetite
- Skin problems
- Mouth sores
- Eye inflammations
What are the causes of ulcerative colitis ?
Scientists suspect that ulcerative colitis may be the result of an overactive body’s immune system. It is unclear why some immune systems react by attacking the huge intestinal tracts and others do not.
Causes that can contribute to developing ulcerative colitis are:
- Genes: You may have inherited a gene from your mother and father that increases your chance of developing ulcerative colitis.
- Various other autoimmune diseases: If you already have one type of autoimmune disease your chances of getting a second one are higher
- Environmental causes: Microorganisms, viruses and antigens can affect your immune system.
What are the risk factors of ulcerative colitis ?
Many people with ulcerative colitis have no family history of the disease. About 12 percent of people with ulcerative colitis have a family member with the disease, according to a 2014 study.
Ulcerative colitis can occur in people of any origin, but it is more common in white people. If you are of Ashkenazi Jewish descent, you have a higher risk of getting the problem than most other groups.
In adolescents with IBD, acne may occur in parallel. Some older research studies have recommended a possible link between taking the cystic acne medication isotretinoin (Absorbica, Amnesteem, Claravis) and ulcerative colitis. However, more recent studies have not yet found a definite causal relationship.
What methods can be used to diagnose ulcerative colitis ?
Several tests can help a doctor diagnose ulcerative colitis. Ulcerative colitis mimics other bowel diseases such as Crohn’s disease. A doctor will do several tests to rule out various other problems.
Investigations to detect ulcerative colitis often include:
- Blood tests: Blood tests are usually helpful in the medical diagnosis of ulcerative colitis. A complete blood count is used to find evidence of anaemia (a low red blood cell count). Other tests indicate inflammation, such as a high level of healthy C-reactive protein and a high blood sedimentation level. A doctor can also buy special antibody tests.
- Stool examination: A doctor will examine your stool for certain inflammation, blood, bacteria and bloodsuckers.
- CT scan: This is a special X-ray examination of your abdomen and pelvis.
- Endoscopy: A doctor uses a flexible tube to examine your stomach, oesophagus and small intestine.Biopsy. A cosmetic surgeon takes a piece of cell from your colon for analysis.
- Flexible sigmoidoscopy: Adaptable sigmoidoscopy is a type of endoscopy. In this examination, a doctor inserts a long, adaptable tube into your anus to examine it, the sigmoid colon and part of the descending colon. Flexible sigmoidoscopy is also known as sigmoidoscopy.
- Colonoscopy: During a colonoscopy, a doctor inserts a lighted endoscope, called a colonoscope, into your anus to take a look inside your colon. It is also a type of endoscopy.
What is a colonoscopy ?
Medical professionals may perform a colonoscopy to detect ulcerative colitis or to determine the severity of the problem. Before the procedure, a doctor will probably instruct you to reduce solid food and switch to an all-liquid diet. You will fast for a period of time before the procedure.
Normal preparation for colonoscopy includes taking a laxative the night before the procedure. This helps to remove any waste that is still in the colon and anus. The doctors can better examine an emptied colon.
During the procedure you will lie on your side. Your doctor will give you a sedative to help you relax and avoid pain. When the medicine has taken effect, the doctor will insert a colonoscope into your anus. This instrument is long and flexible so that it can be moved around comfortably in your gastrointestinal tract. The colonoscope is also equipped with a camera so that your doctor can see the inside of your colon.
During the examination, the doctor looks for signs of swelling and looks for precancerous lesions called polyps. The doctor may also perform a biopsy. The cells may be sent to a research laboratory for further examination.
If you have been diagnosed with ulcerative colitis, your doctor may perform regular colonoscopies to monitor swelling, damage to your bowel and the progress of your recovery.
A colonoscopy is an important tool for detecting bowel cancer cells. Learn why it is so important for people diagnosed with ulcerative colitis.
When should you see a doctor ?
If you have been diagnosed with ulcerative colitis, you should consult a doctor if you experience symptoms such as the following:
- Extreme stomach problems or cramps
- extreme anal bleeding
- Chronic diarrhoea that is difficult to manage
- high fever
- Inflammation in places like the skin or joints
- Dehydration
These signs and symptoms are occasionally associated with difficulties in ulcerative colitis.
If you have not yet been diagnosed with ulcerative colitis, you should see a doctor if you have several signs and symptoms of the disease. He can help you find out if you have ulcerative colitis or another bowel disease.
What are the conventional medical treatment options for ulcerative colitis?
Ulcerative colitis is a stubborn disease. The aim of therapy is to reduce the inflammation that causes your symptoms in order to avoid relapses and achieve longer periods of remission.
1. Medicines
The medication you will take will depend on your individual circumstances, including how severe your symptoms are.
Ulcerative colitis is treated with 2 different medicines: Aminosalicylates (5-aminosalicylic acid, 5-ASA, active ingredient: mesalazine) and corticosteroids.
In addition, drugs that weaken the task of the body’s own immune system can positively influence the course of the disease. These so-called immunosuppressants include azathioprine, methotrexate or cyclosporin A, for example.
2. Hospitalisation
If your signs are severe, you will need to be hospitalised to treat the effects of dehydration and electrolyte loss caused by the diarrhoea. You may also need to have blood replaced and other problems treated.
Researchers are looking for brand new treatments every year.
3. Surgical treatment of ulcerative colitis
Surgical intervention is necessary for:
- significant blood loss
- Persistent and debilitating signs and symptoms
- Opening of the colon
- severe constipation
A CT scan or colonoscopy can reveal these serious problems.
Surgical treatment usually involves removing the entire colon and anus and creating a new pathway for the faeces. This path can be through a small opening in the abdominal wall.
To pass the faeces over the abdominal wall, the doctor will make a tiny opening in the abdominal wall. The end of the lower part of the small intestine, called the ileum, is then brought to the surface of the skin. Through the hole, the stool flows directly into a bag.

In other operations, the doctor removes the diseased part of the colon and rectum, but leaves the outer muscle mass of the rectum intact. The doctor then connects your small intestine to the anus to form a small pouch.
In certain treatments, the anus is also removed.
What is the course & prognosis of ulcerative colitis ?
Ulcerative colitis occurs in episodes: In people over 80, episodes of inflammation alternate with episodes without inflammation. Doctors call this “persistent attacks” or “chronic attacks”. Between episodes, the inflammation subsides and the mucous membranes recover (remission).
Some sufferers have only one outbreak and remain asymptomatic for many years. In about 10 percent of patients, the inflammations do not completely subside after an outbreak.
In some patients, ulcerative colitis starts suddenly with bloody diarrhoea and severe abdominal pain. Those affected have a high fever, are dehydrated and can go into shock. Around 30 per cent of sufferers die during this “fulminant” course.
People with ulcerative colitis have a higher risk of developing colon cancer than healthy, fit people. Whether a colitis patient develops colon cancer depends on the duration of the disease and the severity of the colon disease. After 1,520 years of illness, about eight people develop colon cancer.
In colitis patients who have had their colon completely removed, the small intestinal reservoir (“pouch”) in the rectum can become irritated (pouchitis). The inflammation of the pouch causes diarrhoea, intestinal bleeding and fever. About 30 people have had surgery for pouchitis in 2 years, and up to 50 people have had swelling afterwards. Some people develop chronic pouchitis. Patients are given antibiotics or corticosteroid injections to reduce the inflammation.
Can ulcerative colitis lead to complications ?
Ulcerative colitis increases the risk of developing colon cancer. The risk of developing colon cancer is greater the longer you have had the disease.
Because of this increased risk, your doctor will perform a colonoscopy and screen you for cancer if you are diagnosed.
After that, repeat screenings are recommended every 1 to 3 years, according to the American Cancer Society. Normal screening helps reduce your risk of colorectal cancer cells. Follow-up exams can detect precancerous lesions early.
Other difficulties of ulcerative colitis consist of:
- Enlargement of the intestinal wall surface
- Bleeding in the intestinal tract
- Sepsis or blood infection
- severe dehydration
- toxic megacolon, or a rapidly swelling colon
- Rupture of the colon
- Swelling of the skin, joints and eyes
- Ankylosing spondylitis (Bekhterev’s disease), which causes swelling of the joints between the bones of the spine
- Kidney stones
- Liver disease, which is rare
The problems of ulcerative colitis get worse if the disease is not treated effectively.
Ulcerative colitis in children
According to a study of CED in the US, one in 1,299 children aged 2 to 17 were affected by the problem in 2016. Crohn’s disease was twice as common as ulcerative colitis, and children were also more likely to be affected by IBD than women.
Children with IBD are more likely to be diagnosed at the age of ten. The signs and symptoms of ulcerative colitis are similar in them as in older people. Children may have bloody diarrhoea, abdominal pain and cramps, and fatigue.
In addition, they may have problems that are made worse by the condition, such as:
- Anaemia as a result of blood loss
- Malnutrition due to poor digestion
- unexplained weight loss
Ulcerative colitis can have a significant impact on a child’s life, especially if the disease is not adequately treated and managed. Treatment options for children are particularly limited due to potential complications. For example, medicinal enemas are rarely used as a therapeutic procedure in children.
However, children with ulcerative colitis may be recommended medications that both reduce inflammation while protecting against immune system attacks on the colon. In some children, surgery may be required to treat the signs and symptoms.
If your child has been diagnosed with ulcerative colitis, it is important that you work closely with the doctor to find therapies and lifestyle changes that can help.
11 Tips for ulcerative colitis – What you can do yourself
A number of drug treatments are available for the treatment of ulcerative colitis. The aim of conventional medical treatment is to avoid relapses and to prolong the time between relapses (remission), at least for a short time.
These drugs can have serious side effects, especially when taken over a long period of time. For example, corticosteroids can cause a number of cosmetic, emotional and also hormonal problems.
Many patients simply cannot tolerate these medicines. Children in particular can have problems with basic medications. Because of the negative side effects often associated with taking conventional ulcerative colitis medications, many people are turning to alternative treatments as well as all-natural solutions to manage their ulcerative colitis.
Dietary supplements and herbal remedies for ulcerative colitis
1. probiotics
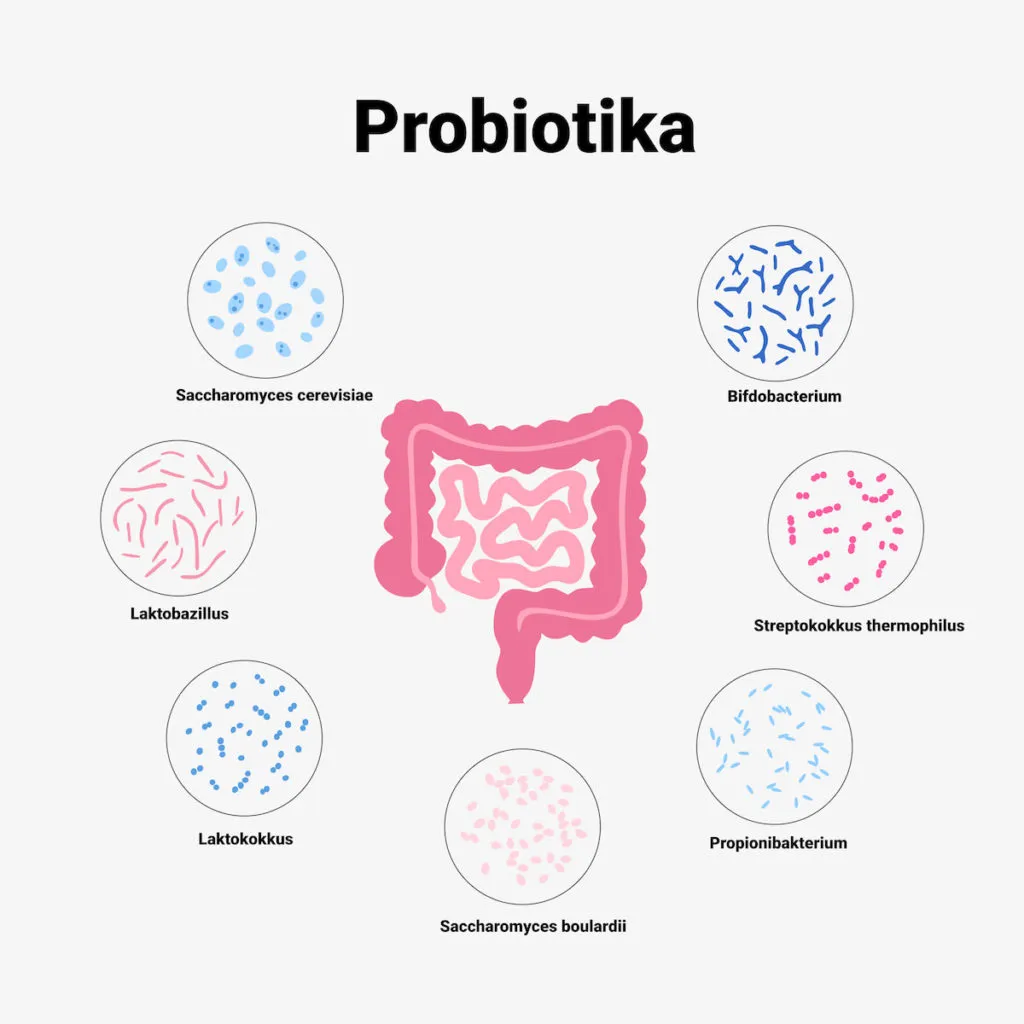
Probiotics provide healthy and balanced gut bacteria to restore and maintain the natural microbial flora in the gut. This can reduce harmful inflammatory responses and maintain remission.
2. ginseng
Although there is a lack of human studies investigating the effect of ginseng on ulcerative colitis, some animal studies have shown that ginseng may be effective in treating ulcerative colitis by reducing swelling and protecting against cell damage.
3. psyllium
Psyllium increases intestinal mobility, relieves symptoms of constipation and improves the elimination of waste.
4. Boswellia
There is evidence that the resin extracted from boswellia plants can help reduce inflammation, which may be practical for people with ulcerative colitis.
5. Bromelain
Bromelain, an enzyme found in pineapples, may help relieve ulcerative colitis symptoms and reduce the frequency of flare-ups. It is a proteolytic enzyme, which means it helps break down proteins.
Bromelain has been shown to reduce inflammation of the intestinal tract and improve cellular function of the digestive system, which may help reduce ulcerative colitis symptoms.
6. Turmeric
Turmeric extract, the Indian spice used in curries, can help people with ulcerative colitis.
In particular, the curcumin found in turmeric is antioxidant and has been shown to reduce inflammation while improving the effectiveness of standard medical therapy.
7. Gingko biloba
Gingko has been shown to be effective in the treatment of experimental colitis in rats.
8. Nutritional measures in ulcerative colitis
For some people with ulcerative colitis, a change in diet can help. A relatively high percentage of people of European descent are allergic or sensitive to gluten, a substance found in wheat.
There is evidence that people with ulcerative colitis are more likely to have coeliac disease or gluten intolerance. Further investigations are needed here.
Avoiding the following foods and drinks could also reduce the regularity and intensity of the episodes:
- Alcohol
- Dairy products
- Meat
- refined food
- carbohydrate-rich foods
- Sugar alcohols
A low-fat diet seems to be particularly useful in delaying the recurrence of ulcerative colitis. Olive oil, medium-chain triglycerides, omega-3 fatty acids and certain dietary fibres may have a beneficial effect.
A high fibre intake can also be helpful for some people. Not only can they improve the regularity of bowel movements, but also the consistency of the stool.
High vitamin C consumption can have a safety-promoting effect, and vitamin C-rich foods may be associated with a longer remission period. These foods include, but are not limited to:
- Berries
- Spinach
- Paprika
- Parsley
9. Diet plan
There is no specific diet for ulcerative colitis. Everyone reacts differently to foods and drinks.A few general guidelines may be useful for people trying to prevent a flare-up:
- Eat a low-fat diet. It is not clear why a low-fat diet plan is useful, but it is known that high-fat foods generally cause diarrhoea, especially in people with IBD.
- Consume more vitamin C. This vitamin could have a protective effect on your bowel and help it recover or regenerate more quickly after an outbreak. People who eat a diet rich in vitamin C take longer to get rid of ulcerative colitis. Foods rich in vitamin C include parsley, peppers, spinach and also berries.
- Eat more fibre. During a disease flare-up, big, slow-moving fibre is the last thing you want in your gut. However, in remission, fibre can help keep you eating regularly. They can also help you to eliminate waste products more easily during bowel movements.
10. Keep a food diary
Keeping a food diary is a smart way to identify which foods affect you. Carefully track what you eat and how you feel in the hours afterwards for several weeks. Record information about bowel movements or other signs and symptoms you experience.
During this period, you are likely to notice fluctuations between discomfort or abdominal pain, as well as certain problematic foods. Remove these foods from your menu to see if your symptoms increase.
You can relieve moderate symptoms of ulcerative colitis by avoiding foods that upset your gastrointestinal tract. Discover the foods that are likely to trigger problems in ulcerative colitis.
11. Lifestyle changes in ulcerative colitis
Ulcerative colitis causes a range of signs and symptoms, not just those of the stomach. In addition to medication, various other treatments as well as lifestyle changes, such as the following, can help improve health and well-being as well as quality of life:
- Treat anaemia immediately. Reduced levels of iron, folic acid and vitamin B-12 can cause anaemia. Reduced iron levels can result from blood loss. Some medicines can interfere with folate absorption. In addition, a vitamin B-12 deficiency may develop. When ulcerative colitis flares up, it can be difficult to get all the nutrients you need. The cause of the anaemia must always be recognised and treated immediately.
- Managing anxiety. Emotional stress is strongly associated with ulcerative colitis. Avoid relapses with the help of stress-reducing exercises or treatments, yoga and reflection.
- Exercise and stop smoking cigarettes. Additional exercise and also regular exercise can help with ulcerative colitis. Can quit smoking cigarettes.
- Discontinue your medication regimen. Certain medications such as non-steroidal anti-inflammatory drugs (NSAIDs) may be associated with ulcerative colitis flare-ups. If you have ulcerative colitis, consult your doctor before taking an NSAID.
The tip at the end
Taking natural remedies together with standard therapies can eliminate the signs of ulcerative colitis much better than conventional therapies alone.
Before you start any alternative treatment, you should talk to your doctor about which remedies are best for you. He or she can help you find the best treatment for you.
Most of these natural solutions can be used together with various other ulcerative colitis treatments. Discover which remedies are risk-free for you and what questions to ask your doctor.
FAQ
Below are some common questions about ulcerative colitis that sufferers ask.
What is the difference between ulcerative colitis and Crohn’s disease?
Ulcerative colitis and Crohn’s disease are the most typical forms of inflammatory bowel disease. Both problems are thought to be caused by an overactive immune system.
They also have many signs in common, consisting of the following:
- Pain
- Abdominal pain
- Diarrhoea
- Fatigue
Nevertheless, there are clear differences between ulcerative colitis and Crohn’s disease. Knowing the main differences can help you make a correct diagnosis.
Localisation
These two problems affect different parts of the gastrointestinal tract
Crohn’s disease can affect any part of the gastrointestinal tract, from the mouth to the anus. It often occurs in the small intestine. Ulcerative colitis only affects the large intestine (colon) and rectum.
Therapy measures
Comparable medications are prescribed to treat both problems. Surgery is also an alternative treatment. It is a last option for both conditions, but can provide a cure for ulcerative colitis, whereas it is only a temporary treatment for Crohn’s disease.
Is ulcerative colitis curable?
Currently, there is no non-surgical cure for ulcerative colitis. Treatment of the inflammatory disease aims to prolong the duration of remission and alleviate flare-ups.
For people with extreme ulcerative colitis, palliative surgery is a treatment option. Removal of the entire colon (as in a total colectomy) can eliminate the symptoms of ulcerative colitis.
This treatment requires your doctor to place a bag outside your body into which the waste can be emptied. This bag can become irritated and cause adverse effects.
For this reason, some people opt for a partial colectomy. In this surgical procedure, the doctor removes only the parts of the colon that are affected by ulcerative colitis.
While these surgical treatments can help relieve or stop the signs of ulcerative colitis, they can also bring unfavourable consequences and possible long-term problems. Read more about these problems to find out if surgery is an alternative for you.
Can you catch ulcerative colitis?
Ulcerative colitis cannot be transmitted.
Some causes of colitis or inflammation in the colon can be transmissible. These include inflammation caused by microorganisms or viruses.
Nevertheless, ulcerative colitis is not caused by something that can be transmitted to another person.
What is an ulcerative colitis flare-up?
A relapse is when ulcerative colitis is active. When a relapse occurs, treatment can help relieve the signs and symptoms and put the body back into a state of remission. Remission is a period of time when the disease is inactive.
During remission, you will not experience any symptoms of ulcerative colitis. However, you will probably need to take regular medication to minimise the possibility of relapses. Numerous days, months or even years may pass between relapses.
Ulcerative colitis can progress and gradually affect other parts of your colon. If ulcerative colitis affects large parts of your colon, you may regularly experience more attacks than someone who has a milder form of the problem.
Do I need a special doctor?
Especially in Europe, inflammatory bowel diseases such as Crohn’s disease or ulcerative colitis are on the rise, which is why an EU-funded project got to the bottom of the immune reactions that trigger these diseases.
The EU-MIRA project study is timely, as the incidence of inflammatory bowel disease (IBD) in Europe is the highest in the world (for reasons that remain unclear), according to the results of a study published in The Lancet: Norway has the highest incidence of ulcerative colitis associated with anal bleeding (505 people per 100,000 population), and Germany also has the highest incidence of Crohn’s disease (322 patients per 100,000 population).
Inflammatory digestive health problems like ulcerative colitis and Crohn’s disease affect 3 million people in the US, according to 2015 data from the Centers for Illness Control and Avoidance (CDC). While this may seem like a large variety, it is a small enough group that not every medical professional has the expertise to treat the problem.
Proctology or coloproctology is a clinical specialty that deals with the diseases of the anus, more specifically the colon, rectum and anal canal. A specialist who deals with proctology is called a proctologist.
A gastroenterologist specialises in treating problems that affect the digestive tract. His experience and practice in dealing with ulcerative colitis will be of use to you in finding the best treatment programme.
What is life with ulcerative colitis like?
Persistent diseases like UC can take up a large part of daily life. Even mild symptoms can be uncomfortable.
Help is available. Support systems for people with UC exist in different areas.
Your doctor or your medical facility’s training centre can help you find the support you need.
ICD codes for this disease: K51 | K51.0 | K51.1 | K51.2 | K51.3 | K51.4 | K51.5 | K51.8 | K51.950
ICD codes are internationally valid codes for medical diagnoses. They can be found, for example, in doctors’ letters or on certificates of incapacity for work.
The web content of ÁYIO-Q.com is for your information and in no case replaces a personal consultation or treatment by a qualified physician. The contents of ÁYIO-Q.com cannot and must not be used to make independent diagnoses or for self-medication.
Sources:
- Herfarth HH, Martin CF, Sandler RS, Kappelman MD, Long MD. Prevalence of a gluten-free diet and improvement of clinical symptoms in patients with inflammatory bowel diseases. Inflamm Bowel Dis. 2014;20(7):1194-1197. doi:10.1097/MIB.0000000000000077
- Seong MA, Woo JK, Kang JH, et al. Oral administration of fermented wild ginseng ameliorates DSS-induced acute colitis by inhibiting NF-κB signaling and protects intestinal epithelial barrier. BMB Rep. 2015;48(7):419-425. doi:10.5483/bmbrep.2015.48.7.039
- Catanzaro D, Rancan S, Orso G, et al. Boswellia serrata Preserves Intestinal Epithelial Barrier from Oxidative and Inflammatory Damage. PLoS One. 2015;10(5):e0125375. Published 2015 May 8. doi:10.1371/journal.pone.0125375
- Zhou Z, Wang L, Feng P, et al. Inhibition of Epithelial TNF-α Receptors by Purified Fruit Bromelain Ameliorates Intestinal Inflammation and Barrier Dysfunction in Colitis [published correction appears in Front Immunol. 2017 Dec 13;8:1769]. Front Immunol. 2017;8:1468. Published 2017 Nov 10. doi:10.3389/fimmu.2017.01468
- Yan-Hong Zhou, Jie-Ping Yu, Yi-Fei Liu, Xiao-Jun Teng, Mei Ming, Peng Lv, Ping An, Shi-Quan Liu, Hong-Gang Yu, “Effects of Ginkgo biloba Extract on Inflammatory Mediators (SOD, MDA, TNF-α, NF-κBp65, IL-6) in TNBS-Induced Colitis in Rats“, Mediators of Inflammation, vol. 2006, Article ID 092642, 9 pages, 2006. https://doi.org/10.1155/MI/2006/92642
- Ammon HP. (2010). Modulation of the immune system by Boswellia serrata extracts and boswellic acids. DOI:10.1016/j.phymed.2010.03.003
- Ke F, et al. (2012). Herbal medicine in the treatment of ulcerative colitis. DOI:
- Baliga MS, et al. (2012). Curcumin, an active component of turmeric in the prevention and treatment of ulcerative colitis: Preclinical and clinical observations. DOI: 10.1039/c2fo30097d
- Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies, auf https://www.thelancet.com/, Zugriff 07.01.2022