Updated on 9. June 2022 from Carolin Jäger
Reading time: approx. 15 minutes
Everything you need to know about hives at a glance
Urticaria, as the medical term is known, is a widespread skin disease that affects people all over the world. The disease is colloquially called hives. Experts estimate that one in four adults between the ages of 20 and 40 will suffer from urticaria at least once in their lifetime. Approximately 800,000 people in Germany are affected by chronic urticaria. The restriction of the quality of life and the ability to work is sometimes considerable.
Who treats urticaria and is hives contagious? What can you do about it yourself? You can find answers to questions like these and many more in the following article.
- Types
- Symptoms
- Causes
- Trigger
- Possible concomitant diseases
- Conventional medical treatment
- 11 Naturopathic therapies & home remedies
What is hives?
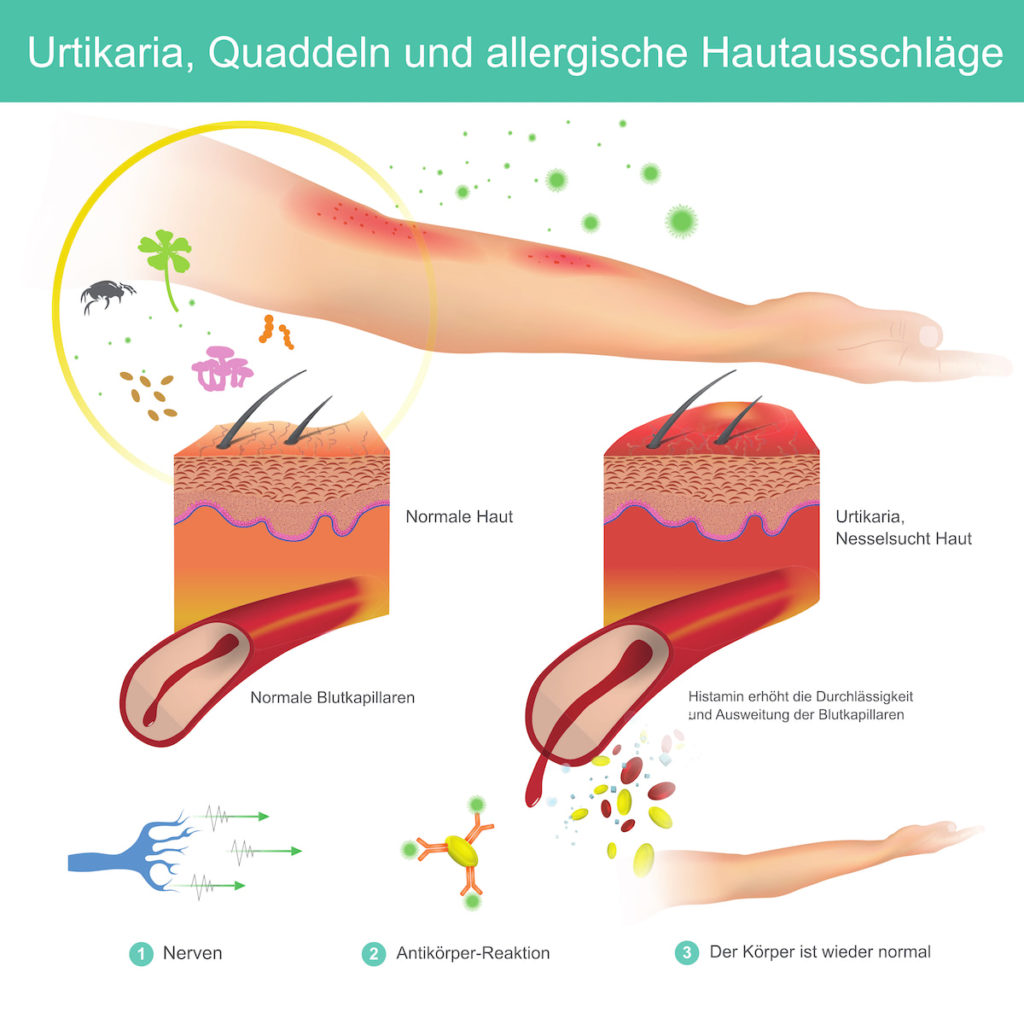
Although the term is less well known, the often distressing symptoms of hives, which can affect anyone, include sudden redness on the skin followed by bright red to bright red bumps.
These so-called wheals can vary in size, from the size of the palm of your hand to the head of a pin, and they itch like crazy. The wheals collect with fluid. The person often feels a burning and tightening sensation on the skin.
Urticaria is named after the symptoms that occur when the skin comes into contact with nettle (Latin: urticaria). However, the symptoms can also occur without warning and without a known cause. For most people, the rash disappears after a few days. For many people, however, the hives return year after year and affect their entire lives.
Hives – Where does it occur?
The localisation of the skin disease on the body varies from patient to patient.
Hives most commonly occur on the following areas of the body:
- Face
- Neck
- Hands
- Elbows
On the other hand, patients with urticaria on the feet are not special. Urticaria symptoms also often occur in areas where clothing is too tight and chafes. Hives can also be a rash that can affect the whole body (generalised urticaria).
Hives – An allergy?
Hives are a type of allergic reaction that occurs when the body is exposed to certain stimuli. Doctors therefore call it a “pseudoallergy”. A pseudoallergic reaction to medicines or food can play a role in the development of the rash.
An “actual” allergic reaction is almost never the cause of urticaria.
Urticaria has many faces

Hives (urticaria) is a skin rash (exanthema) characterised by itchy wheals and in some cases swelling of the skin and/or mucous membranes. Urticarial skin reactions can be triggered by a variety of events.
The localisation of the skin disease on the body varies from patient to patient. Urticaria symptoms also often occur in regions where clothing is too tight and chafes. Generalised urticaria is a rash that can affect the entire body.
Depending on the intensity and duration of the symptoms, hives can be extremely stressful on a person’s life and can significantly affect daily activities.
What are the types of hives?
Urticaria can be classified according to many different factors. The most common classifications are:
- Acute urticaria (less than 6 weeks)
- Chronic urticaria (more than 6 weeks)
- Undefined spontaneous urticaria
- Ill-defined physical urticaria
- Undefined “other types” of urticaria
Hives are often categorised according to the source of the rash.
Hives can come in different shapes and sizes. They do not usually occur at the same time. Some people have two or more of these forms of the disease at the same time.
The types of hives can be divided into three categories:
1. Spontaneous hives
Hives and/or angioedema occur without warning or external stimuli. About 80 per cent of all urticaria patients present with idiopathic urticaria, two-thirds of which are acute urticaria.
2. Physical hives
All types of hives that are triggered by physical stimuli fall into this category (e.g. pressure, wind, cold contact, etc.). Only about ten percent of all hives cases are caused by them.
3. Other forms of hives, for example due to:
- Physical activity
- Contact with water
- Perspiration
Only about ten percent of all hives patients suffer from this type of hives.
Is hives contagious?
Definitely – Not! Infection is not possible. The skin disease is not dangerous for other people because it cannot be transmitted by contact.
Hives – The typical symptoms
Hives (urticaria) have clear symptoms that are easy to recognise. Nevertheless, almost two thirds of those affected have no idea what causes the terrible itching, swelling and wheals on the skin.
Itching that is excruciating
Hives are one of the most annoying skin diseases, because they are characterised by a burning itch (lat. pruritus) that feels as if it has been caused by contact with a stinging nettle. The itching often has serious effects on patients and leads to lack of sleep and difficulty concentrating at work. Almost everyone who suffers from hives has an uncontrollable urge to scratch. Chronic urticaria is often accompanied by psychiatric disorders such as sadness or anxiety and, in the worst cases, suicidal thoughts. Translated with www.DeepL.com/Translator (free version)
Formation of wheals
The sudden reddening of the skin followed by bright red elevations, sometimes called wheals, is one of the classic hives symptoms. These itchy, wandering swellings of the upper and middle dermis are clearly visible and palpable and may be accompanied by a burning sensation.
The wheals can be as small as pinheads, as large as a coin or as large as the palm of a hand. The wheals are limited to small areas of skin in moderate cases, but can spread to large areas of skin in more severe cases. The wheals usually resolve within 24 hours and leave no scars or signs. However, they may reappear on another part of the body.
Angioedema – When the skin swells up
An angioedema, a sudden and painful swelling of the deeper layers of the skin (lower dermis and subcutis), is also a possibility. The huge, fuzzy, deep swellings that characterise angioedema can be recognised. In some hives patients, this symptom occurs at the same time as the itching and wheals, but may last for several days.

Angioedema develops in only a few patients. Deep swellings often occur on the face, head, neck and arms. It is particularly unpleasant when the eyelids or lips swell up so much that the affected person can no longer work and does not dare to leave the house. Angioedema can cause life-threatening shortness of breath if it affects the airways and larynx.
In the acute stage of the disease, the hives symptoms usually disappear on their own within a day. The symptoms of chronic urticaria, on the other hand, can last for years or recur over and over again.
Hives – When to see a doctor?
If you get itchy welts on your skin, you should keep an eye on the rash. You should see a doctor if the symptoms last longer than 24 hours.
Your family doctor is the best person to talk to when you first see a rash. He or she can recognise your symptoms and refer you to a dermatologist if necessary. If you already know you have hives, you should see your dermatologist if you notice any changes in your skin.
If the hives are accompanied by fever, you should definitely consult a doctor. It is possible that an acute infection is the cause.
Hives – What are the causes?
What is the origin of hives? This is a question many patients ask themselves, but it is difficult to answer. The development of hives is a complicated process:
When certain immune cells (mast cells) are irritated, they produce messenger substances that increase inflammation and lead to an itchy rash. One of these messenger substances is the tissue hormone histamine, which is primarily responsible for the symptoms of hives (wheals, itching, skin redness, swelling).
But what causes the mast cells to become irritated? It may be an allergic reaction (to certain foods, pollen, etc.). Mast cells are also triggered in many other circumstances in different ways. This shows that not all hives are caused by an allergic reaction.
Hives – What are the typical triggers?
Urticaria can occur in different forms, each with its own triggers. These triggers, in turn, are often difficult to determine. What all forms have in common is that they are not inherited. The most common triggers for hives are listed below.
Spontaneous hives:
- It is usually triggered by an illness and can last up to two weeks.
- Food
- Medications
Physical hives:
- Pressure
- Increase in body temperature/cold
- Water
Other forms of hives:
- Effort
- Contact
Hives and anaphylaxis
Anaphylaxis is a life-threatening allergic reaction that can spread throughout the body.
It can cause severe breathing problems and unconsciousness. If not treated immediately, it can be fatal. This is a life-threatening situation.
You should consult a doctor immediately if you experience any of the following symptoms:
- Vomiting and nausea
- Cold and clammy skin fast heartbeat fainting or light-headedness an unexpected, sudden feeling of great anxiety swelling of the mucous membranes of the mouth, tongue, lips and throat, causing difficulty breathing
- Anyone suffering from hives should look out for other symptoms that may indicate an anaphylactic reaction.
Hives – Possible concomitant diseases
Hives can be a strong opponent, especially if it is unclear what is causing the itchy, red wheals that appear all over the body and can last up to six weeks. One reason could be a hidden disease. Chronic hives have been linked in studies to autoimmune diseases such as thyroid disease, rheumatoid arthritis, celiac disease, type 1 diabetes, Sjögren’s syndrome and lupus.
Hives as a result of autoimmunity
Although an allergic reaction can trigger hives, the cause remains unknown in some people. “Chronic spontaneous urticaria” is the name for this condition. Some of these chronic hives patients may have autoimmune urticaria, which is hives caused by an autoimmune reaction to different antigens in the body.
Studies suggest that up to 40% of people with persistent idiopathic hives have an autoimmune disorder. Scientists are still piecing together the puzzle, but it is thought that excessive amounts of autoantibodies are responsible. These are the harmful antibodies of the immune system that interfere with the body’s own functions. It is also known that women are affected more often than men.
Hives and autoimmune thyroid disease
The most common autoimmune disease associated with persistent hives is autoimmune thyroid disease. This link has been studied by scientists for decades. In thyroid disease, commonly called autoimmune thyroiditis, the body produces antibodies that target the thyroid gland. Compared to a control group of adults who did not have hives, some patients with a history of persistent hives had significantly higher levels of thyroid antibodies. Unfortunately, action against these antibodies is only indicated when there is also an imbalance of thyroid hormones. Although there is a link between thyroid antibodies and the occurrence of hives, it is unclear whether these antibodies are the cause of the hives.
Chronic hives, hyperthyroidism and hypothyroidism
hyperthyroidism or hypothyroidism of the thyroid gland can be caused by autoimmune thyroiditis. Chronic hives may be caused by any of the following: Irritability, muscle weakness, sleep disturbances, rapid heartbeat, sensitivity to heat, diarrhoea, trembling of the hands and weight loss are all symptoms of hyperthyroidism. Hypothyroidism causes hypothyroidism, which can manifest itself in sensitivity to cold, lethargy, constipation, depression, weight gain, hair loss and dry skin.
Chronic hives in rheumatoid arthritis
In people with persistent hives, rheumatoid arthritis is the second most common autoimmune disease.
Rheumatoid arthritis occurs when the body’s immune system attacks the joints and thickens the tissue that lines the inside of the joints. People suffering from this inflammatory autoimmune disease are at increased risk of a number of skin problems, including recurrent hives. According to one study, female patients with persistent hives were more likely to be diagnosed with rheumatoid arthritis.
Chronic hives are associated with rheumatic factors
Compared to control groups, rheumatoid factors, proteins produced by the immune system that target healthy tissue in the body, were found to be much more prevalent in people with chronic hives. Symptoms of rheumatoid arthritis include painful, swollen joints and nodules, as well as hard lumps under the skin and numerous skin rashes.
Celiac disease and hives
Coeliac disease patients have an increased risk of developing chronic hives, according to a large-scale study. When coeliac patients consume gluten, a protein found in wheat, barley and rye, their immune system attacks their small intestine. To treat the symptoms of this inherited autoimmune disease, sufferers must avoid gluten. Painful bloating, recurrent diarrhoea, constipation, vomiting and exhaustion are possible symptoms.
Celiac disease and hives are linked
According to one study, hives are 1.5 times more common in people with coeliac disease. Under certain circumstances, patients can be diagnosed with hives first and then coeliac disease. According to the researchers, coeliac disease is the cause of almost one-third of cases of chronic hives. Women are more likely to develop coeliac disease.
Diabetes is associated with autoimmune diseases as well as persistent hives
People with type 1 diabetes, like people with other autoimmune diseases, are more likely to develop other autoimmune diseases such as coeliac disease or thyroid disease, as well as chronic hives. According to studies, children who initially presented with persistent hives were later diagnosed with autoimmune thyroid disease and eventually type 1 diabetes. In another example, an adult with type 1 diabetes and Graves’ disease developed persistent hives out of nowhere.
Lupus and chronic urticaria
Lupus studies have found a link between lupus and chronic hives, and persistent hives can sometimes be the first sign of the disease. Lupus is an autoimmune disease that can damage joints, skin, kidneys, blood cells, brain, heart and lungs, among other things. A butterfly-shaped rash on the face and both cheeks and rashes on other parts of the body are the most characteristic signs. As with other autoimmune diseases, nine out of ten patients with autoimmune diseases are women.
Hives occur in about ten percent of lupus patients. Individual wheals subside and disappear within a few hours, while new wheals appear. Individual wheals that persist for more than 24 hours may be caused by lupus-related inflammation of the blood vessels.
Treatment of hives with conventional medicine
In most cases, the body heals itself and the hives do not recur (acute urticaria). Chronic urticaria, on the other hand, lasts a long time and can recur, so therapy is crucial. The triggers must be avoided as much as possible to achieve a symptom-free life.
The following medicines are used for this purpose:
- Antihistamines are medicines used to treat allergies (e.g. cetirizine).
- Combination with cortisone after 2-3 days: takes effect within 24 hours
- In particularly severe cases, ciprofloxacin can be used. It inhibits the immune system (immunosuppressant), but needs 10-14 days to take effect.
11 Naturopathic Therapies & Home Remedies for Hives
1. Complaints diary
Hives can be triggered by a variety of chemicals or irritants, and it can be difficult to identify the triggering substances or irritants. However, the best treatment is to avoid potential triggers. Keeping a careful log of symptoms can help detect hidden triggers. Hives can be treated with home remedies to relieve symptoms and improve quality of life. If you have a chronic form of urticaria that lasts longer than six weeks, you should see a dermatologist. If you experience symptoms such as difficulty swallowing or shortness of breath, you should seek emergency medical attention immediately.
2. Cold treatments
Many sufferers find that cool compresses, a cool shower or applying cooling gels to the skin are very soothing. Adding a chamomile or peppermint infusion to a compress helps to soothe inflamed skin. A calming effect on hives symptoms can be achieved by taking a short, cool, full bath with baking soda or baking powder. Cooling is of course not the best treatment for people with cold urticaria!
3. Bowel cleansing for hives
Intestinal cleansing, also known as symbiosis therapy, is a home remedy for hives that can relieve the symptoms. More than 400 different species of bacteria form a healthy intestinal flora that regulates the immune system and, among other things, prevents pathogens from spreading in the intestines, pollutants from entering and diseases from developing. The two goals of intestinal cleansing are as follows: On the one hand, intestinal cleansing aims to help normalise the part of the immune system located in the intestinal mucosa. On the other hand, intestinal cleansing aims to rebuild the intestinal mucosal barrier to prevent adverse reactions to food components. The symbiosis is controlled with specially produced microbes (probiotics) that are taken regularly. Bifidobacteria and lactobacilli are used in particular.
Treatment with a probiotic can be particularly useful if urticaria sufferers have had to take antibiotics more frequently in the past or if food intolerances have been identified as the cause of the symptoms. Since there are so many different probiotics with different bacteria, it is best to seek advice from a doctor or pharmacist to find the preparation that is right for you.
4. Medicinal plants for the treatment of hives

5. Calcium for the treatment of urticaria, itching and wheals
Calcium is safe for mild to severe hives (urticaria) and can be used if there are no known contraindications. Given the diversity of urticaria types, it is logical that there is no one-size-fits-all dose for calcium.
In a randomised, placebo-controlled double-blind study on pollen allergy sufferers in the prick test with a product containing organically bound calcium, a statistically significant reduction of the wheal area could be convincingly documented; which is further evidence for the anti-allergic effect of calcium in sufficient dosage.
6. Vitamin D and hives
A metastudy concluded that the urticaria population, especially adult chronic urticaria patients, are at risk for low serum 25(OH)D levels. Vitamin D may be useful in the treatment of chronic urticaria as an immune enhancer and anti-inflammatory agent. According to the study, vitamin D supplementation reduces the severity of urticaria while improving overall quality of life.
Read our detailed article on Vitamin D.
7. Vitamin C and hives
Vitamin C is also said to have a positive effect on hives. Classical medicine recommends about 1000mg of vitamin C per day, naturopathy about 8000mg per day distributed over several single doses, which has a similar effect as an antihistamine.
Read our detailed article on Vitamin C.
8. Wine vinegar for hives has a calming effect
Wine vinegar is another home remedy for hives. It is important to discuss with your doctor whether it can be used or not.
The pH value of the skin, i.e. the acidity, is regulated by wine vinegar. This influences how efficiently the skin’s acid mantle works. Hives irritate the skin, and skin with a regulated pH is better prepared for them.
A lukewarm bath can contain wine vinegar. Applying diluted wine vinegar (one tablespoon of vinegar to one litre of water) to the inflamed skin can also help. The skin can become dry with this treatment.
9. Natron (soda bicarbonate – baking powder)
Baking soda in combination with water can help relieve itching. Use the powder on your skin or when bathing with water.
10. Zinc

Zincal ointment is a common home treatment for hives in children. It soothes the skin and supports the healing process.
11. Stress prevention
- Meditation
- Autogenic training
- Relaxation exercises
- Breathing exercises
In addition, it is important to drink enough high-quality water every day and not to neglect detoxification (liver cleansing) and deacidification of the body.
Hives – When psychological tension invades the skin
According to another study, stress is an important risk factor for the development of chronic idiopathic urticaria, while positive coping tendencies and good family support seem to have a preventive effect. Insomnia may be the most important psychosomatic symptom that is a predisposing factor for chronic urticaria.
Psychological stress can cause a variety of symptoms. Stress-induced hives show the usual signs of a skin disease: Redness of the skin, wheals and severe itching.
The skin reaction may be limited to a small area of skin or may extend over a larger area. It is also conceivable that deeper swelling (angioedema) may occur.
If the swelling affects the throat, for example, and makes breathing difficult, this can have fatal consequences. In these cases, and if the itching and wheals persist for six weeks or longer, a dermatologist should be consulted immediately.
In severe and extremely stressful disease situations, the connection between hives and the psyche can have psychosocial consequences: In the case of severe hives on the skin, the psychological stress symptoms also increase, which can possibly lead to psychological sequelae such as depression.
The acute itching that occurs in chronic hives in recurrent and unexpected episodes is a great burden that greatly affects the quality of life and makes it difficult to keep appointments or appointments.
As a result, some patients become increasingly isolated and avoid contact with other people. Anxiety and stress become the focus of their lives, putting a strain on the psyche and can exacerbate the hives.
Both the physical symptoms and the stress need to be treated to break this vicious circle.
Stress causes hives because histamine is produced
The immune system is damaged by psychological stress. Avoiding internal turbulence therefore serves as a preventive measure. Stress, like all other irritants that are recognised as triggers, should be avoided in hives.
Histamine can aggravate the irritation and lead to the formation of wheals, which further aggravates the skin condition.
Therefore, dermatologists take a comprehensive approach to their patients. They look for allergens as probable triggers, but also take into account the patient’s psychological state, especially in severe relapses.
Doctors refer to stress-induced urticaria as a condition in which psychological stress is associated with wheal formation. For sufferers, the following applies: In addition to skin problems, underlying stress should also be addressed. This includes analysing circumstances or disputes at work or in private life that are associated with high psychological stress and avoiding them if possible.
Hives: Avoiding stress can help relieve symptoms
Is it possible to avoid psychological stress altogether? It is not always possible. However, it is possible to treat stress and reduce its prevalence in everyday life. To do this, techniques must be found that enable the hives symptoms caused by stress to be reduced more quickly as a therapeutic strategy.
Since stress arises so that the organism can react quickly, intuitively and efficiently to serious events that threaten the existence – which, however, are rare nowadays – the inner turmoil needs relief.
Hives – What can I do?
Stress reduction as well as the “right attitude” towards your skin are the be-all and end-all of treatment from a psychological point of view. Try to find out the reasons why you suffer from hives.
The ÁYIO-Q Centre of Vitality offers various solutions. Among other things, stress can be eliminated within a few minutes with the help of ÁYIO-Q Pnoē-Therapy. Stress can be eliminated within a few minutes. If you would like to know more about your vital energy and the state of your self-healing powers, it is best to take the free self-test on our website.
(Note: As an Amazon affiliate, we earn on qualifying sales)
FAQ
What foods can trigger hives?
Hives can be an allergic reaction to certain foods, and some allergy sufferers get hives after eating them. Hives can be triggered by a variety of foods, including cow’s milk, almonds, fish and chicken eggs. Some people are allergic to certain foods just by touching them. This can happen when cooking or preparing meals, for example. Food, on the other hand, is rarely the cause of hives.
Foods with a high histamine content can trigger symptoms in people who are not allergic to them. Histamine from food is normally broken down during digestion, but in certain people it is absorbed into the bloodstream, causing acute urticaria.
Urticaria is a side effect of some people’s reactions to food supplements. Sweeteners such as aspartame and colourings and flavourings are examples. Pseudoallergies are reactions that have nothing to do with an actual allergy.
Is it true that homeopathy can help with hives?
Globules, which are small balls of highly diluted chemicals used in homeopathy, are used in both naturopathy and homeopathy for a variety of problems. They can relieve the symptoms of urticaria. Some homeopaths also use nettle extract to cure patients who have a chronic condition. This is injected into the muscle regularly for a few weeks. There is no scientific proof of efficacy for this therapy, but it seems to help certain people.
Is it possible to exercise if you suffer from hives?
Physical exertion, especially sport, is the cause of symptoms in some people. However, it is not advisable to avoid sports, as regular exercise offers several health benefits. In such cases, the doctor will prescribe an antihistamine, which the sufferer should take immediately before exercise to avoid any effects.
Can I swim despite my hives?
Some people get cold urticaria as a reaction to the cold. For them, it is best to stay out of the cold, which includes swimming. This is because extremely cold water or even a rapid cooling of the skin after swimming can trigger the symptoms.
Can I go to the sauna if I have hives?
In heat urticaria, some people develop hives when they have too much Can hives be fatal?
Urticaria, whether acute or chronic, is unpleasant but harmless if it only affects the skin. The skin changes usually disappear by themselves after some time. Some people may also have angioedema (swelling of the skin) on the face or lips. This can be very painful and uncomfortable. If the tongue or palate is affected, it can cause serious breathing problems. It can also be life-threatening if other symptoms such as tiredness, shortness of breath or coughing occur after an allergic reaction. In this case, it is essential to consult a doctor.
Why does hives usually appear in the evening?
For many patients, the symptoms appear out of the blue. Such itching episodes occur more frequently in the evening and at night and often affect the quality of life of those affected. This is because the symptoms are compounded by lack of sleep and fatigue during the day. However, it is unclear why the symptoms manifest themselves mainly in the evening and at night.
What should you do if your child has hives?
You should closely monitor a child who suffers from itchy wheals, i.e. urticaria symptoms. It is important to contact a paediatrician if the wheals do not disappear quickly, if the child appears impaired, if he or she has additional symptoms or if the wheals reappear. If such skin changes are accompanied by swelling of the cheeks and lips, it can become dangerous: Immediate treatment is required! This also applies if an allergic reaction causes severe, possibly life-threatening symptoms.heat. A visit to the sauna will almost always lead to itchy skin lesions, which should be avoided.
Sources:
[1] Hives, at https://www.nesselsuchtinfo.de/, accessed 04.12.2021
[2] Nettis E, Foti C, Ambrifi M, et al. Urticaria: recommendations from the Italian Society of Allergology, Asthma and Clinical Immunology and the Italian Society of Allergological, Occupational and Environmental Dermatology. Clin Mol Allergy. 2020;18:8. Published 2020 May 6. doi:10.1186/s12948-020-00123-8
[3] The most frequently asked questions at a glance, at https://www.urtikaria.net/, accessed 04.12.2021
[4] Zuberbier T, Aberer W, Asero R, et al. The EAACI/GA(2) LEN/EDF/WAO Guideline for the definition, classification, diagnosis, and management of urticaria: the 2013 revision and update. Allergy. 2014;69(7):868-887. doi:10.1111/all.12313
[5] Chronic urticaria and autoimmunity: Associations found in a large population study, auf https://www.jacionline.org/, Zugriff 04.12.2021
[6] Chronic spontaneous urticaria and autoimmunity: a follow up study of patients with chronic urticaria for 16 years, auf https://www.jacionline.org/, Zugriff 04.12.2021
[7] Syndrome of idiopathic chronic urticaria andangioedema with thyroid autoimmunity: A
study of 90 patients, auf https://www.jacionline.org/, accessed 04.12.2021
[8] Nuzzo V, Tauchmanova L, Colasanti P, Zuccoli A, Colao A. Idiopathic chronic urticaria and thyroid autoimmunity: Experience of a single center. Dermatoendocrinol. 2011;3(4):255-258. doi:10.4161/derm.3.4.17066
[9] Kim DH, Sung NH, Lee AY. Effect of Levothyroxine Treatment on Clinical Symptoms in Hypothyroid Patients with Chronic Urticaria and Thyroid Autoimmunity. Ann Dermatol. 2016;28(2):199-204. doi:10.5021/ad.2016.28.2.199
[10] Ludvigsson JF, Lindelöf B, Rashtak S, Rubio-Tapia A, Murray JA. Does urticaria risk increase in patients with celiac disease? A large population-based cohort study. Eur J Dermatol. 2013;23(5):681-687. doi:10.1684/ejd.2013.2158
[11] Celiac Disease Prevalence in Women, auf https://www.beyondceliac.org/, Zugriff 04.12.2021
[12] Chronic urticaria and autoimmunity: Associations found in a large population study, auf https://www.jacionline.org/, Zugriff 04.12.2021
[13] Mazzetti A, Borici-Mazi R. Childhood chronic urticaria and type 1 diabetes. Allergy Asthma Clin Immunol. 2011;7(Suppl 2):A18. Published 2011 Nov 14. doi:10.1186/1710-1492-7-S2-A18
[14] Autoimmune chronic urticaria associated with type 1 diabetes and Graves’ disease, at https://www.jacionline.org/, accessed 04.12.2021
[15] Sjögren-Syndrom, auf https://www.niams.nih.gov/, accessed 04.12.2021
[16] Spadoni M, Jacob C, Aikawa N, Jesus A, Fomin A, Silva C. Chronic autoimmune urticaria as the first manifestation of juvenile systemic lupus erythematosus. Lupus. 2011;20(7):763-766. doi:10.1177/0961203310392428
[17] Lupus-Specific Skin Disease and Skin Problems, at https://www.hopkinslupus.org/, accessed 04.12.2021
[18] Website of ECARF – European Centre for Allergy Research Foundation. http://www.ecarf.org/info-portal/erkrankungen/urtikaria/. Accessed 04.12.2021.
[19] Maurer M, Weller K, Bindslev-Jensen C, et al. Unmet clinical needs in chronic spontaneous urticaria. A GA²LEN task force report. Allergy. 2011;66(3):317-330. doi:10.1111/j.1398-9995.2010.02496.x
[20] Angioödem, at http://www.angiooedem.net/. Accessed 04.12.2021
[21] Tips and tricks – alleviate discomfort, at http://www.urtikaria.net/, accessed 04.12.2021.
[22] K. Widhalm, M. Miklautsch: Ernährungsmedizin: mit 219 Tabellen. Deutscher Ärzte-Verlag, Cologne, 2009, p. 484f.
[23] White Paper, Allergy in Germany. 2nd updated and enlarged edition, Urban und Vogel (2004).
[24] Schöpf E., Czech W., Mueller J, Allergiebehandlung mit Calcium? / Fragen aus der Praxis; MMP, 19.Jg, Heft 2, 56 (1996).
[25] Li Y, Cao Z, Guo J, Li Q, Su J. Effects of Serum Vitamin D Levels and Vitamin D Supplementation on Urticaria: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health. 2021;18(9):4911. Published 2021 May 5. doi:10.3390/ijerph18094911
[26] Yang HY, Sun CC, Wu YC, Wang JD. Stress, insomnia, and chronic idiopathic urticaria–a case-control study. J Formos Med Assoc. 2005;104(4):254-263.
[27] Sánchez-Borges M, Ansotegui IJ, Baiardini I, et al. The challenges of chronic urticaria part 1: Epidemiology, immunopathogenesis, comorbidities, quality of life, and management. In: World Allergy Organ J. 2021;14(6):100533
[28] Memet B, Vurgun E, Barlas F, Metz M, Maurer M, Kocatürk E. In Chronic Spontaneous Urticaria, Comorbid Depression Linked to Higher Disease Activity, and Substance P Levels. In: Front Psychiatry. 2021 May 26;12:667978.
[29] Tzur Bitan D, Berzin D, Cohen A. The association of chronic spontaneous urticaria (CSU) with anxiety and depression: a nationwide cohort study. In: Arch Dermatol Res. 2021;313(1):33-39.