Updated on 10. March 2022 from ÁYIO-Q Redaktion
Reading time: approx. 20 minutes
Time for action – When the heart loses its power
Many people, especially older people, suffer from heart failure. The disease affects physical and mental health as well as well-being. Unfortunately, this complex, intractable disease is often underestimated.
The numbers often come as a shock: the impact of heart failure is severe worldwide. It affects around 26 million people worldwide and also leads to more than 1 million hospitalisations per year in the United States and Europe (as of 2014).
What is heart failure and how exactly does it develop? How is it diagnosed and treated and how can you prevent and counteract heart failure?
- Description
- Shapes & Stages
- Symptoms
- Causes & Risk-factors
- Diagnose
- Conventional treatment
- Disease progression & Prognosis
- Natural & alternative therapy options
What happens in heart failure ?
According to the World Health Organisation (WHO) definition, heart failure is a syndrome (typically a mixture of accompanying signs) of breathlessness and fatigue associated with cardiovascular disease. To understand what heart failure is, you need to understand the heart and its function.
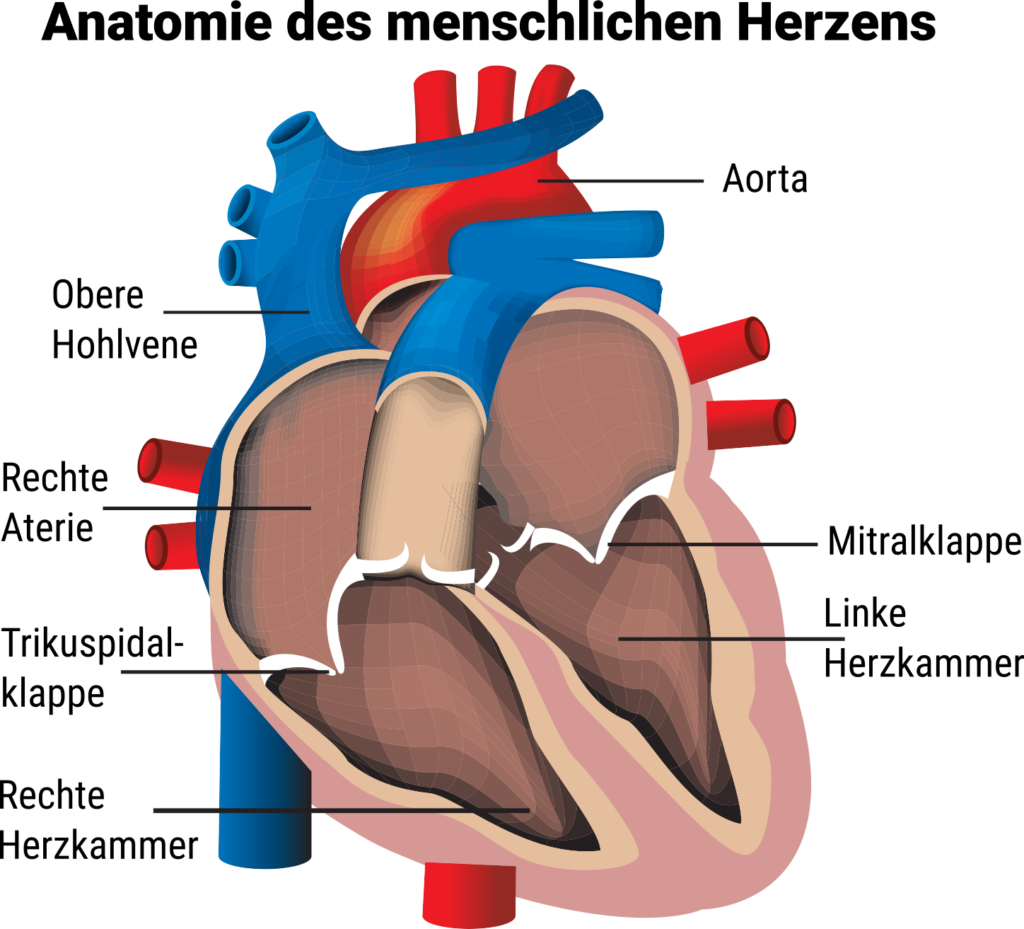
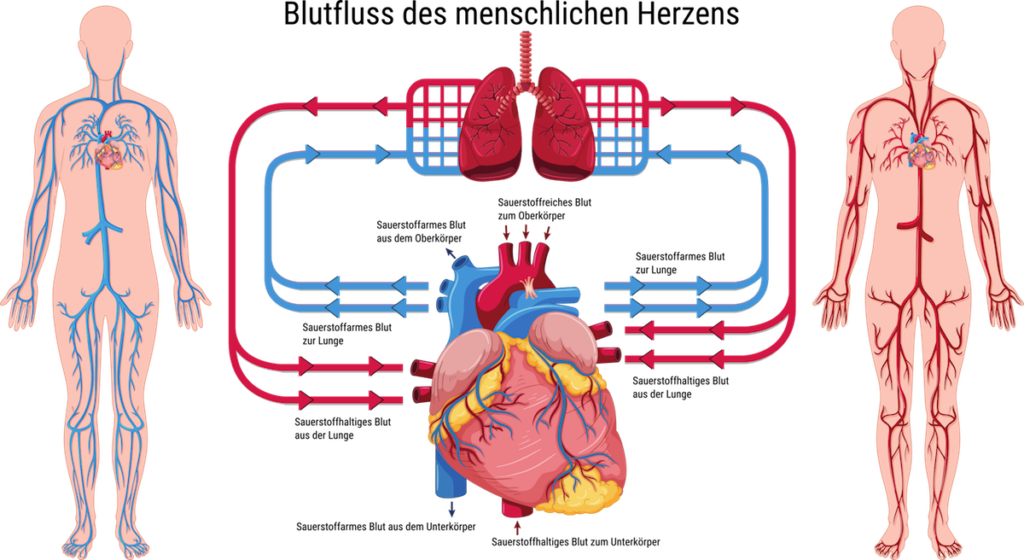
The heart consists of a left and a right hemisphere and is also the basis of the circulatory system. A healthy heart pumps oxygen-rich blood into the blood vessels via the left half of the heart. After it has passed through the body, the now deoxygenated blood returns to the heart. Via the right side of the heart, the blood flows into the lungs, where it is oxygenated again and the cycle begins anew.
With heart failure, the prognosis for the heart is poor. Years of high blood pressure or coronary artery disease, in which deposits of cholesterol and other fats narrow the coronary arteries, can be responsible.
On the one hand, heart failure signals to the organism that the available blood is not being pumped completely through the body. As a result, the organs of the body are undersupplied with oxygen and nutrients, which they need quickly according to their characteristics. On the other hand, the heart cannot fully absorb the incoming blood. Therefore, cardiovascular disease can have serious effects not only on the heart, but on all organs of the body.
Very often heart failure occurs together with many other diseases, also called comorbidities. Not only the treatment of heart failure, but also the treatment of the comorbidities is important.
What are the different forms and stages of heart failure?
Depending on whether it is left-sided heart failure or right-sided heart failure, the signs are different. Both sides of the muscle can also be affected, in which case doctors speak of generalised heart failure.
Depending on this, retrograde or antegrade circulatory failure occurs:
- Reverse failure: When blood flows from both the body and the lungs to the heart. The tension in the blood vessels increases, allowing fluid to enter the cells. This often occurs in vertical cardiac arrest and can lead to fluid build-up in the body, for example in the feet, legs or abdomen, among other things.
- Forward failure: This means that the ejection port of the heart is not sufficient to supply the body with enough blood. The amount of oxygen reaching the body and organs is much less, so shortness of breath and weakness may occur. This condition often occurs in left-sided heart failure.
In addition to this classification of heart failure, cardiologists also use the New York Heart Foundation (NYHA) table to assess the severity of heart muscle weakness. A distinction is made between the following four stages:
NYHA phase I: Heart failure without physical limitation. Everyday physical exertion does not produce any discomfort of any kind.
NYHA stage II: Heart failure with moderate limitation. No pain at rest and little physical exertion. Symptoms of dyspnoea or arrhythmia on exertion, e.g. walking uphill or climbing stairs.
NYHA phase III: Heart failure with higher degree of limitation: No symptoms at rest. Symptoms such as shortness of breath or cardiac arrhythmia with low exertion, e.g. when walking.
NYHA phase IV: Heart failure with signs on physical exertion and also at rest: Affected persons are usually bedridden.
What are the symptoms of heart failure?
The signs and symptoms of incipient heart failure are often non-specific. Early medical diagnosis is usually difficult, and distinguishing it from other causes of the disease is also not always easy.
If heart failure persists, the heart’s pumping capacity slowly decreases. The first signs and symptoms of heart failure are a drop in performance, shortness of breath and also weight gain. Severe heart failure is much more dramatic.
The following list can help you recognise the common signs:
1. Shortness of breath (dyspnoea) – a typical sign of left-sided heart failure
Dyspnoea can occur, on the one hand, when the heart does not transport the blood completely and the blood backs up in the lungs. On the other hand, a damaged heart can no longer meet the increased demand of the muscles, especially during physical exertion. The lack of oxygen and other nutrients in the muscles leads to rapid exhaustion, which the affected person perceives as shortness of breath or muscle weakness.
2. Reduced performance and also rapid fatigue
Many people with heart failure literally feel tired very quickly, but also mentally exhausted. This is because sufferers usually worry about their health and fear that they will no longer be able to manage daily life independently.
3. Difficulty sleeping
Several patients with heart failure struggle with breathing pauses during rest (central sleep apnoea). Breathing suddenly stops completely for a few seconds (in severe cases for several minutes). The result: the body is no longer supplied with enough oxygen. As a direct result of this resting apnoea, the body increases the work of the heart in order to compensate for the lack of oxygen through faster blood circulation; high blood pressure and heart rate increase. Over a short period of time, the heart can normally still perform this task. Over time, however, the pressure can become too great.
4. Dizziness / Fainting
Your condition and sometimes the medication you are taking can cause dizziness and/or impaired thinking.
5. Water retention (oedema) – in right-sided heart failure
When the body stores water, swelling of the ankles, feet, legs or abdomen can occur. These are all typical symptoms of heart failure. In addition, rapid weight gain occurs due to the retained water.
6. Persistent cough – in left-sided heart failure
Heart failure is often accompanied by incessant coughing or hissing. These problems are another effect of the accumulation of fluid in the lungs.
7. Fair, cool skin
The decreasing pumping capacity of the heart can significantly reduce blood flow to the skin. Regular signs are paleness, cold skin as well as an increased sensitivity to cold.
8. Blocked throat capillaries
Blockage of the neck capillaries is said to occur when the veins on the right and left sides of the neck are clearly visible when the patient is at rest or standing. In the case of severe venous congestion in the neck, the veins at the base of the tongue may also be blocked.
9. Accelerated pulse, especially on exertion (“palpitations”)
10. Accelerated breathing (in left-sided heart failure)
11. Rattling/whistling sounds when breathing (in left-sided heart failure)
12. Weight gain
13. Nocturnal urge to urinate
Acute heart failure: signs and symptoms within minutes
Unlike chronic heart failure, the signs and symptoms of acute heart failure occur unexpectedly, within minutes or hours. Due to a heart attack, extreme high blood pressure or other heart disease, the heart’s performance suddenly drops sharply.
What are the causes and risk factors of heart failure?
In heart failure (cardiac insufficiency), the heart is no longer as efficient as a healthy heart. Heart failure can develop for a number of reasons:
One of the most common causes of heart failure is calcification of the coronary arteries (coronary artery disease, CAD). Calcified plaques cause the vessels that supply the heart muscle to become narrowed and blood can no longer flow through them properly. As a result, the heart muscle is undersupplied and is no longer as reliable.
With high blood pressure, the heart has to pump harder and harder, for example against narrowed vessels in the bloodstream. Over time, the heart muscle mass thickens to be able to build up the extra load (Hypertrophy).
Other causes of heart failure are cardiac arrhythmias and inflammation of the heart muscle. Problems with the cardiac septum as well as (genetically determined or acquired) heart valve defects can also lead to heart failure. The same applies to fluid accumulation in the pericardium (pericardial effusion, especially in Pericarditis).
Heart failure can also be caused by heart muscle diseases (cardiomyopathies). In this disease, also called Tako-Tsubo cardiomyopathy, the heart function usually returns to normal. So there is no irreversible heart failure.
Metabolic diseases can also play a role in the development of heart failure. Examples are diabetes mellitus (diabetes) and thyroid function disorders (e.g. hyperthyroidism = overactive thyroid gland).
Diseases of the lungs such as emphysema or COPD (chronic obstructive pulmonary disease) are other possible causes of heart failure. In particular, the much rarer right heart failure (functional weakness of the right side of the heart) can be caused by lung disease.
In some people, heart failure develops as a result of anaemia or disease in other organs of the body, such as liver or kidney disease. In rare cases, an AV fistula (AV shunt) causes heart failure. This is an unusual short-circuit connection between an artery and a vein.
Sometimes medicines also trigger heart failure. This risk exists, for example, with certain medicines for cardiac arrhythmias, certain cancer medicines (antineoplastic medicines), appetite suppressants and also migraine medicines (such as ergotamine). Heart nodules or metastases of cancer cells can also cause heart failure.
Which methods can be used to diagnose heart failure?
To diagnose heart failure, the doctor will first ask about signs and symptoms and your medical background. If the GP thinks you have heart failure, he or she should refer you to a cardiologist for further investigations.
Detect heart failure with ultrasound and ECG

The ultrasound examination can, for example, provide information about whether the heart muscle mass is enlarged, the heart chambers are larger or the heart valves are not functioning properly.

The ECG result can provide evidence of coronary artery disease and, if necessary, show whether the person has suffered an undetected heart attack.
What are the conventional medical treatment options for heart failure?
Conventional medical therapy for heart failure is primarily aimed at improving the quality of life of those affected and also reducing mortality, i.e. increasing life expectancy in terms of the overall prognosis. Unfortunately, drug treatment of heart failure with controlled pump function (HFpEF) has little or no success compared to heart failure with impaired pump function (HFrEF).
Treatment for persistent heart failure aims to slow the progression of the disease and increase life expectancy and quality of life. When choosing the right treatment for you, your doctor will certainly take into account the underlying disease that led to the heart failure and the intensity of the signs and symptoms present.
Standard therapy for heart failure includes several elements:
1. Treatment of the underlying disease
If there is a causal underlying disease, it may have to be treated. This includes, for example, diseases of the coronary vessels or cardiac arrhythmias.
2. Non-drug treatments
This includes, among other things, that the patient adheres to a healthy lifestyle and is thoroughly educated about his or her disease.
3. Medicines
A number of medicines are used to treat heart failure. The medicines help to relieve and also protect the heart.
- ACE inhibitors are mainly prescribed for high blood pressure, but also for chronic heart failure. They dilate the capillaries and thus ensure that the blood pressure is lowered and the heart is relieved.
- Medicines with a dual action: Angiotensin receptor neprilysin inhibitors (ARNIs) are a mix of drugs containing both an angiotensin receptor blocker and a neprilysin inhibitor. ARNIs are suitable for people with a certain type of heart failure. They can both calm the heart and favourably influence the programme of the disease.
- Drugs to slow down the heartbeat: Beta (receptor) blockers interfere with the regulation of the tension hormones adrenaline and noradrenaline. Therefore, the hormonal substances are restricted in their effect, which makes the heart failure more regular.
- Medicines to stabilise the heart rhythm: Digitalis preparations or cardiac glycosides are obtained from the foxglove, a medicinal plant. They strengthen the pumping action of the heart, but are being used less and less. Doctors recommend them mainly for cardiac arrhythmias or atrial fibrillation.
- Diuretics: To support the heart in its function, doctors often recommend diuretics. They have a diuretic effect and thus also support the therapy of heart failure. In advanced heart failure, so-called aldosterone antagonists are also used. They are also called potassium-saving diuretics because of their diuretic effect. Another effect of the drugs is that they reduce the accumulation of connective tissue around the heart caused by the body’s own hormone aldosterone. The aldosterone level can be permanently elevated, for example due to high blood pressure. This subsequently promotes the increased formation of connective tissue cells, making the heart stiffer and stiffer.
4. Cardiac resynchronisation therapy
In patients with severe heart failure (as well as proven iron deficiency) who continue to have symptoms despite optimal drug therapy, so-called resynchronisation therapy by pacemaker stimulation in the right as well as left ventricle can be carried out under certain conditions to improve the symptoms and also the diagnosis. This type of therapy is usually combined with the implantation of a cardioverter/defibrillator to protect those affected from fatal arrhythmias. Recently, however, the implantation of a defibrillator has proven to be somewhat more prudent when the heart failure is not caused by coronary artery disease.
5. Surgical measures
In the presence of vasoconstriction due to coronary artery disease, blood flow in the coronary arteries can be improved by vasodilation (balloon dilatation with possible insertion of a stents) or coronary bypass. In cases of extreme valve damage, surgical treatment with valve reconstruction or replacement with an organic or mechanical valve prosthesis is required.
Heart transplantation is a last but firmly established form of therapy for severe heart failure, as it improves the survival rate, resilience and also the quality of life of these severely ill people compared to conventional therapy. Artificial hearts or so-called ventricular assist devices can be used to bridge the waiting period until heart transplantation.
The results of the last ten years show a survival rate of 85 % after the first year of transplantation and a 5-year survival rate of about 70 %. Heart transplantation requires intensive post-operative treatment and extensive therapy with putative immunosuppressants to prevent rejection.
- The goal of all heart failure therapies is to relieve the signs of heart failure. In many cases, consistent treatment of heart failure helps patients to lead active lives despite their heart failure.
What is the course & prognosis of heart failure
Heart failure cannot be cured. Only in a few cases can the symptoms be reduced to such an extent that a completely unencumbered life is possible. However, each individual can influence whether and how far the disease progresses. By changing their lifestyle and consciously dealing with the disease, those affected can contribute a great deal to improving their prognosis.
Life expectancy and the quality of life of individuals have increased in recent years due to increasingly better medical treatment. Patients today have a better prognosis and a relatively long life expectancy, regardless of the disease. In individual cases, this depends on the type (genesis) of the disease, the age of the person affected, possible concomitant diseases and the individual lifestyle.
12 tips for heart failure – What you can do yourself
If your doctor has diagnosed you with heart failure, it is necessary to maintain a healthy and balanced lifestyle. This will certainly reduce the dangers and increase your quality of life. For this reason, you should take the following advice to heart:
1. Preparation of a diet plan
Make sure you eat a diet with plenty of fruit and vegetables. Avoid animal fats as much as possible and eat a low-salt diet. Salt causes water to be stored in the body. As a result, the heart has to work harder.
2. Monitoring fluid intake
You need to talk to your doctor about the amount of fluid you need to drink every day. Fluid intake. As a general rule, you should never drink 3 litres or more a day if you have heart failure. Most of the time, a fluid intake of about 2 litres per day is ideal.
3. Do sport
Effective treatment of heart failure always includes exercise and moderate physical activity.
Patients with heart failure have long been advised to take it easy and avoid physical exertion. However, many scientific studies have shown that moderate endurance training has a positive effect on heart failure. Exercise is not only safe, but also an important part of treatment.
Exercise in heart failure improves the physical performance and lifestyle of those affected. It is still unclear whether exercise also has an influence on the life expectancy of patients.
A 2018 study from the College of Texas Southwestern found that an exercise programme of at least four to five times a week can help the ageing heart and also prevent heart disease such as heart failure.
A lifestyle change with an increased exercise programme that includes high and moderate intensity exercise is an effective approach to reversing the effects of inactive ageing on the heart.
The Texas researchers note in their study that heart failure is usually preceded by a loss of elasticity in the heart muscle mass. The increased ” stiffness of the heart ” seems to be the result of reduced exercise in midlife.
They suggest the following training strategy:
- 1 hour of cardiovascular training in the fitness centre, walking, playing tennis or cycling 1 time per week
- 1 hour of high impact aerobics 1 time per week
- 1 hour of strength training, 1 time per week
- In addition, strength training 2 to 3 times a week at medium intensity, which means that you sweat throughout the training but can still have fun, which is no longer possible with high strength
You can also join a sports group for heart patients (rehab sports).
Reduce body weight4;
Being overweight has a profound impact on heart failure. Even normal-weight heart failure patients should check their weight regularly, preferably daily. Rule of thumb: If you gain more than one kilo per night, even more than two kilos in three nights or more than 2.5 kilos in one week, you must consult your doctor.
5. Reduce alcohol
Reduce your alcohol consumption, because alcohol can damage the heart muscle cells. Women are recommended to consume no more than twelve grams of pure alcohol (one drink as a criterion) per day. Men should not consume more than 24 grams of pure alcohol (comparable to two regular drinks) per day. Patients whose heart failure was caused by too much alcohol consumption (alcohol toxic cardiomyopathy) must abstain from alcohol completely.
6. Reduce smoking
It is best to give up smoking altogether!
7. Keeping a diary
Keep a diary of any complaints you notice. This way you won’t forget anything the next time you go to the doctor.
8. Traditional Chinese medicine (TCM)
The therapy consists mainly of acupuncture and Chinese phytotherapy. The treatment set-up includes treatment with Chinese phytotherapy, in which formulas are prepared from various herbal active ingredients and then ingested.
9. Naturopathy
First, a thorough laboratory analytical examination should be carried out. This must include one of the most important minerals and micronutrients, vitamins, enzymes, fat and amino acids as well as serious intensity parameters.
In particular, optimal orthomolecular care based on valid laboratory results is crucial for treatment.
For the resolution of minerals and trace elements, the whole blood evaluation must be used, as this allows the intracellular and extracellular mineral amounts to be reliably determined. The parameters to be determined in this way should include magnesium, calcium, potassium, zinc and also selenium.
Various other orthomolecular substances that are crucial for typical cardiac function and also need to be clarified by laboratory diagnostics are coenzyme Q10 (especially when taking statins (cholesterol-lowering drugs)), L-carnitine, L-arginine, taurine, vitamin D, vitamin C, homocysteine, ADMA and, for follow-up, also proBNP.
Only through the optimal supply of all substances needed for the heart muscle mass can the main performance system be permanently increased. If orthomolecular substances are not replenished, a long-term drug-free supply is hardly possible.
Especially in the case of cardiac arrhythmias, at least potassium must be constantly available in the blood as a neuromuscular pacemaker. It is impressive how little attention is paid to this mineral in the signs mentioned above.
Nevertheless, even the therapy plan described above alone does not lead to success for all people, although in many cases a clear improvement can be observed.
10. Soluble peptides
Another treatment option that is recommended is the use of soluble peptides. The first syringes with so-called “fresh cells”, which are no longer allowed to be marketed today, were developed by the Swiss doctor Prof. Dr. Niehans.
The valuable soluble peptides used today are intracellular components of a healthy cell whose cell membrane has actually been completely filtered off and which are also produced under extremely high manufacturing requirements. Notable unfavourable events, such as allergic reactions, are very rarely observed, as these preparations are considered to be basically antigen-free. Basically, the principle of action according to Paracelsus “like cures like” applies.
From application observations, heart insufficiencies and additionally cardiac arrhythmias could be significantly improved with this technique in many cases. The heart failure decreased significantly, the subjective feeling as well as the performance of the affected persons increased and the cardiac arrhythmias detected by ECG measurements decreased or were no longer detected. In many cases, the medication used could be minimised or discontinued.
11. Medicinal plants

Mild to moderate heart failure can be treated very well with natural remedies (NYHA phase I and II). In phases III and IV, naturopathic treatment can accompany conventional medication.
Plants that have a heart-strengthening effect in diluted doses (cardiac glycosides) include:
- Foxglove,
- Lily of the Valley,
- Adonis florets and
- Sea Onion.
They are used to produce various medicines that are also suitable for permanent treatment.
Hawthorn strengthens the heart, promotes blood circulation and additionally acts against cardiac arrhythmia and the risk or signs of coronary heart disease (CHD). The beneficial effect of hawthorn in phase I and II heart failure according to NYHA (New York Heart Organization) has been proven by numerous professional studies and is undisputed.
In addition, there are a number of plants that help to drain oedema.
The well-known aquaretics cat’s beard leaves (Orthosiphonis folium), birch leaves (Betulae folia), nettle leaves (Urticae dioicae folia), goldenrod herb (Solidaginis virgaureae herba) have a diuretic effect.
Field horsetail herb (Equiseti herba), horsetail root (Ononidis radix), or the couch grass rootstock (Agropyri repentis rhizoma), asparagus root (Asparagi rhizoma), pumpkin seeds (Cucurbitae peponis seminal fluid), as well as green tea (Theae viridis folium). Lovage root (Levistici radix), parsley (Petroselini herba and Petroselini radix), currant leaves (Ribis nigri folia) can also be used as supportive agents.
12. Strophanthin provides support in heart failure
If you need drug support during the transition phase – until a dietary change and nutrition programme take hold – strophanthin could help. Strophanthin is a very old heart medication that was used in medical practice until the late 20th century, when it was superseded by normal pharmaceutical antihypertensives and various other heart medications.
Strophanthin, obtained from an African plant, is not only used for heart failure, but also for coronary heart disease, high blood pressure or cardiac arrhythmias.
Tips for prevention
It is good for the body to walk or cycle to work instead of taking the car or public transport. During breaks, you can go out into the fresh air instead of staying in the office.
Getting enough exercise in your free time keeps you balanced and also prevents heart failure. For example, you can have fun with your children or grandchildren (who will certainly appreciate it), get a dog and take it for a walk or join a hiking group or a dance club. In this way, not only is the body sufficiently exercised, but you also make new social contacts, which is very important for your general physical well-being. People who are more than happy get sick much less often than unhappy or dissatisfied people.
FAQ
How dangerous is heart failure?
Heart muscle weakness always requires medical clarification and should not be dismissed as a typical symptom of old age. It is important to start treatment quickly. Among other things, this can minimise the risk of thrombosis or water retention, so-called oedema.
Working with heart failure: Is this feasible?
In principle, heart failure does not prevent you from continuing to do your job. The decisive factors are the stage of the disease, the nature of your job and the assessment of the cardiologist treating you. Often the doctor will suggest a period of rest, for example after a cardiovascular disease. Take advantage of this time, e.g. during rehabilitation at the institution, and find out about all the necessary applications that are important for reintegration into work. To do this, you must contact the health insurance fund and also the pension insurance institution, among others.
Can I fly at all with heart failure?
The oxygen content in the air is much lower in aeroplanes. This is not a problem for patients with well-monitored and stable heart failure, so they do not usually need to be offered supplemental oxygen. Nevertheless, you should talk to your doctor again before travelling.
It is also advisable to contact the airline and find out about the regulations for taking medicines with you. If your bag is lost en route, a safety supply in your hand luggage can help in some cases. Your doctor can additionally provide you with a certificate, if required by the airline, allowing you to take medication with you when travelling with heart failure.
Is driving a car with heart failure possible?
Many people with heart failure assume that they should not drive, but this is not the case. There is a risk of signs and symptoms such as arrhythmia or drowsiness, the ideal medication lowers these signs and symptoms of heart failure. This means that patients with heart failure can also drive. The prerequisite is that the medication is taken as recommended and regularly – adherence to therapy is crucial.
How does heart failure affect my mind and memory?
People with heart failure experience a number of signs and symptoms related to the reduced blood supply to the brain: for example, drowsiness, mood swings and memory problems. Heart failure also has a strong effect on the subconscious – anxiety can be the result of the condition.
What should I avoid when eating with heart failure?
A heart-healthy diet plan must above all contain as few unhealthy fats as possible. These consist of unsaturated fatty acids, such as those found in red meat or fast food. Vegetable fats, on the other hand, which are saturated, can be consumed.
With heart failure – how much can I drink?
Those affected must not drink too much, but they must drink enough. About two litres of fluid a day is a guideline. Your cardiologist can give you more precise information.
What else is important in heart failure besides a healthy and balanced diet?
A balanced diet for the heart is essential for people with heart failure. Furthermore, sufficient exercise must be part of the daily programme. In addition, normal check-up visits to the doctor are on the programme after the medical diagnosis.
Do I need to see a doctor if I have heart failure?
One thing is certain: only a doctor is able to diagnose heart failure with certainty. As a general rule, if you have any signs, you should first see your family doctor and tell him or her about your uncertainties. He or she will refer you to a heart specialist, called a cardiologist. The specialist has assessment tools with which he or she can determine heart failure.
Before this happens, however, a comprehensive medical history is taken. In the following, the doctor inquires about everything concerning the patient’s medical history – this includes, for example, previous illnesses and concomitant diseases, signs as well as the regular intake of medication.
What can cause heart failure?
The most common causes of heart failure include:
- Hereditary factors
- Coronary heart disease (CHD)
- Cardiac arrest
- Cardiac arrest problems
- Hypertension
- Diabetes mellitus
- Resting apnoea
- Treatment of cancer cells
- Heart muscle inflammation
- Cardiac arrhythmias
- Hyperthyroidism
ICD codes for this condition: I50
ICD codes are internationally valid codes for medical diagnoses. They can be found, for example, in doctors’ letters or on certificates of incapacity for work.
The web content of ÁYIO-Q.com is for your information and in no case replaces a personal consultation or treatment by a qualified physician. The contents of ÁYIO-Q.com cannot and must not be used to make independent diagnoses or for self-medication.
Sources:
- Ambrosy AP, Fonarow GC, Butler J, et al. The global health and economic burden of hospitalizations for heart failure: lessons learned from hospitalized heart failure registries. J Am Coll Cardiol. 2014;63(12):1123-1133. doi:10.1016/j.jacc.2013.11.053
- Medizinreport: Chronic heart failure: The number of patients is increasing, but so are the differentiated therapies, Dtsch Arztebl 2016; 113(25): A-1207 / B-1014 / C-998, auf https://www.aerzteblatt.de/, accessed 05.01.2022
- Theresa A McDonagh, Marco Metra, Marianna Adamo, Roy S Gardner, Andreas Baumbach, Michael Böhm, Haran Burri, Javed Butler, Jelena Čelutkienė, Ovidiu Chioncel, John G F Cleland, Andrew J S Coats, Maria G Crespo-Leiro, Dimitrios Farmakis, Martine Gilard, Stephane Heymans, Arno W Hoes, Tiny Jaarsma, Ewa A Jankowska, Mitja Lainscak, Carolyn S P Lam, Alexander R Lyon, John J V McMurray, Alexandre Mebazaa, Richard Mindham, Claudio Muneretto, Massimo Francesco Piepoli, Susanna Price, Giuseppe M C Rosano, Frank Ruschitzka, Anne Kathrine Skibelund, ESC Scientific Document Group, 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: Developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) With the special contribution of the Heart Failure Association (HFA) of the ESC, European Heart Journal, Volume 42, Issue 36, 21 September 2021, Pages 3599–3726, https://doi.org/10.1093/eurheartj/ehab368
- Howden EJ, Sarma S, Lawley JS, et al. Reversing the Cardiac Effects of Sedentary Aging in Middle Age-A Randomized Controlled Trial: Implications For Heart Failure Prevention. Circulation. 2018;137(15):1549-1560. doi:10.1161/CIRCULATIONAHA.117.030617
- Kristen AV, Schuhmacher B, Strych K, et al. Acupuncture improves exercise tolerance of patients with heart failure: a placebo-controlled pilot study. Heart. 2010;96(17):1396-1400. doi:10.1136/hrt.2009.187930
- Li X, Zhang J, Huang J, et al. A multicenter, randomized, double-blind, parallel-group, placebo-controlled study of the effects of qili qiangxin capsules in patients with chronic heart failure. J Am Coll Cardiol. 2013;62(12):1065-1072. doi:10.1016/j.jacc.2013.05.035
- Pittler MH, Schmidt K, Ernst E. Hawthorn extract for treating chronic heart failure: meta-analysis of randomized trials. Am J Med. 2003;114(8):665-674. doi:10.1016/s0002-9343(03)00131-1
- Hawthorn extract for heart complaints, Experimental and clinical studies, auf https://www.uniklinik-freiburg.de/, accessed 05.01.2022